Biblio du mois : Juin-Juillet 2019
Revue sur le coup de chaleur en été en cette période de canicule !
Mais aussi de plus en plus d’études sur le machine learning pour éventuellement vous libérer du temps pour le prochain Afterbloc ? ou goûter le nouvel ingrédient de médecine traditionnelle chinoise contre les PAVM ?
Pour les plus studieux, voici une biblio du mois bien remplie avec de la hépato/chir dig avec de l’évaluation du TIPS ou du traitement chirurgical des péritonites
Du débat sur l’intérêt de manoeuvres de recrutement sur les complications respiratoires post-opératoires : il semblerait qu’une PEEP seule suffise. Bref, de quoi alimenter vos débats lors de la prochaine pétanque !
Sinon du classique avec de l’infectio (impact des DDS pour relancer le débat), de l’ACR et du pronostic, de la physio avec microcirculation…
Un petit point sur les allergies vu le retard de la pollenisation cette année
Et parce qu’il faut rester en forme l’été, une étude « kétamine bonne mine » en tant qu’anti-dépresseur !
Et n’oubliez pas de participer et de partager notre sondage sur vos déclarations (ou non) des AES : https://fr.surveymonkey.com/r/6QF6NH8
Détection d’activité cérébrale par EEG+machine learning chez les traumatisés crâniens ?
Jan Claassen,et al. N Engl J Med 2019; 380:2497-2505
https://www.nejm.org/doi/full/10.1056/NEJMoa1812757?query=TOC
DOI: 10.1056/NEJMoa1812757
Background
Brain activation in response to spoken motor commands can be detected by electroencephalography (EEG) in clinically unresponsive patients. The prevalence and prognostic importance of a dissociation between commanded motor behavior and brain activation in the first few days after brain injury are not well understood.
Methods
We studied a prospective, consecutive series of patients in a single intensive care unit who had acute brain injury from a variety of causes and who were unresponsive to spoken commands, including some patients with the ability to localize painful stimuli or to fixate on or track visual stimuli. Machine learning was applied to EEG recordings to detect brain activation in response to commands that patients move their hands. The functional outcome at 12 months was determined with the Glasgow Outcome Scale–Extended (GOS-E; levels range from 1 to 8, with higher levels indicating better outcomes).
Results
A total of 16 of 104 unresponsive patients (15%) had brain activation detected by EEG at a median of 4 days after injury. The condition in 8 of these 16 patients (50%) and in 23 of 88 patients (26%) without brain activation improved such that they were able to follow commands before discharge. At 12 months, 7 of 16 patients (44%) with brain activation and 12 of 84 patients (14%) without brain activation had a GOS-E level of 4 or higher, denoting the ability to function independently for 8 hours (odds ratio, 4.6; 95% confidence interval, 1.2 to 17.1).
Conclusions
A dissociation between the absence of behavioral responses to motor commands and the evidence of brain activation in response to these commands in EEG recordings was found in 15% of patients in a consecutive series of patients with acute brain injury.
Comment guider la prise en charge avec la Troponine Ultra-sensible ?
https://www.nejm.org/doi/full/10.1056/NEJMoa1803377?query=TOC
Neumann, et al., N Engl J Med 2019; 380:2529-2540
DOI: 10.1056/NEJMoa1803377
Background
Data regarding high-sensitivity troponin concentrations in patients presenting to the emergency department with symptoms suggestive of myocardial infarction may be useful in determining the probability of myocardial infarction and subsequent 30-day outcomes.
Methods
In 15 international cohorts of patients presenting to the emergency department with symptoms suggestive of myocardial infarction, we determined the concentrations of high-sensitivity troponin I or high-sensitivity troponin T at presentation and after early or late serial sampling. The diagnostic and prognostic performance of multiple high-sensitivity troponin cutoff combinations was assessed with the use of a derivation–validation design. A risk-assessment tool that was based on these data was developed to estimate the risk of index myocardial infarction and of subsequent myocardial infarction or death at 30 days.
Results
Among 22,651 patients (9604 in the derivation data set and 13,047 in the validation data set), the prevalence of myocardial infarction was 15.3%. Lower high-sensitivity troponin concentrations at presentation and smaller absolute changes during serial sampling were associated with a lower likelihood of myocardial infarction and a lower short-term risk of cardiovascular events. For example, high-sensitivity troponin I concentrations of less than 6 ng per liter and an absolute change of less than 4 ng per liter after 45 to 120 minutes (early serial sampling) resulted in a negative predictive value of 99.5% for myocardial infarction, with an associated 30-day risk of subsequent myocardial infarction or death of 0.2%; a total of 56.5% of the patients would be classified as being at low risk. These findings were confirmed in an external validation data set.
Conclusions
A risk-assessment tool, which we developed to integrate the high-sensitivity troponin I or troponin T concentration at emergency department presentation, its dynamic change during serial sampling, and the time between the obtaining of samples, was used to estimate the probability of myocardial infarction on emergency department presentation and 30-day outcomes.
Epidémie actuelle d’Ebola en RDC
Revue sur le « coup de chaud »
https://www.nejm.org/doi/full/10.1056/NEJMra1810762?query=pulmonary
Revue sur la prise en charge des brûlés
https://www.nejm.org/doi/full/10.1056/NEJMra1807442?query=pulmonary
Bolus IV de NaCl 0.9% ou d’Albumine associés à plus de morbi-mortalité en réa péd ?
DOI:https://doi.org/10.1016/S2213-2600(19)30114-6
Background
Methods
Findings
Interpretation
Méta-analyse sur l’extension de la thrombolyse d’AVC à 9h ou au réveil avec l’IRM de perfusion
Campbell et al. Lancet 2019;epublished May 21st
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)31053-0/fulltext
DOI:https://doi.org/10.1016/S0140-6736(19)31053-0
Bénéfice du TIPS précoce chez le patient cirrhotique + rupture de VO ?
Yong Lv, et al., Lancet Gastro 2019
https://www.thelancet.com/journals/langas/article/PIIS2468-1253(19)30090-1/fulltext
DOI:https://doi.org/10.1016/S2468-1253(19)30090-1
Background
Methods
Findings
Interpretation
Hartman ou anatomose en 1 temps pour les péritonites diverticulaires ?
Background
Methods
Findings
Interpretation
Echec des mesures de qualité à améliorer la prise en charge des patients
Peden et al., Lancet 2019
Background
Methods
Findings
Interpretation
Echec de la stratégie haute PEP + manoeuvres de recrutement sur les complications respiratoires post-opératoires chez la patient obèse ?
Importance An intraoperative higher level of positive end-expiratory positive pressure (PEEP) with alveolar recruitment maneuvers improves respiratory function in obese patients undergoing surgery, but the effect on clinical outcomes is uncertain.
Objective To determine whether a higher level of PEEP with alveolar recruitment maneuvers decreases postoperative pulmonary complications in obese patients undergoing surgery compared with a lower level of PEEP.
Design, Setting, and Participants Randomized clinical trial of 2013 adults with body mass indices of 35 or greater and substantial risk for postoperative pulmonary complications who were undergoing noncardiac, nonneurological surgery under general anesthesia. The trial was conducted at 77 sites in 23 countries from July 2014-February 2018; final follow-up: May 2018.
Interventions Patients were randomized to the high level of PEEP group (n = 989), consisting of a PEEP level of 12 cm H2O with alveolar recruitment maneuvers (a stepwise increase of tidal volume and eventually PEEP) or to the low level of PEEP group (n = 987), consisting of a PEEP level of 4 cm H2O. All patients received volume-controlled ventilation with a tidal volume of 7 mL/kg of predicted body weight.
Main Outcomes and Measures The primary outcome was a composite of pulmonary complications within the first 5 postoperative days, including respiratory failure, acute respiratory distress syndrome, bronchospasm, new pulmonary infiltrates, pulmonary infection, aspiration pneumonitis, pleural effusion, atelectasis, cardiopulmonary edema, and pneumothorax. Among the 9 prespecified secondary outcomes, 3 were intraoperative complications, including hypoxemia (oxygen desaturation with Spo2 ≤92% for >1 minute).
Results Among 2013 adults who were randomized, 1976 (98.2%) completed the trial (mean age, 48.8 years; 1381 [69.9%] women; 1778 [90.1%] underwent abdominal operations). In the intention-to-treat analysis, the primary outcome occurred in 211 of 989 patients (21.3%) in the high level of PEEP group compared with 233 of 987 patients (23.6%) in the low level of PEEP group (difference, −2.3% [95% CI, −5.9% to 1.4%]; risk ratio, 0.93 [95% CI, 0.83 to 1.04]; P = .23). Among the 9 prespecified secondary outcomes, 6 were not significantly different between the high and low level of PEEP groups, and 3 were significantly different, including fewer patients with hypoxemia (5.0% in the high level of PEEP group vs 13.6% in the low level of PEEP group; difference, −8.6% [95% CI, −11.1% to 6.1%]; P < .001).
Conclusions and Relevance Among obese patients undergoing surgery under general anesthesia, an intraoperative mechanical ventilation strategy with a higher level of PEEP and alveolar recruitment maneuvers, compared with a strategy with a lower level of PEEP, did not reduce postoperative pulmonary complications.
Epreuve de VS versus CPAP avant extubation
Subirà et al. JAMA 2019;321(22):2175-2182
Importance Daily spontaneous breathing trials (SBTs) are the best approach to determine whether patients are ready for disconnection from mechanical ventilation, but mode and duration of SBT remain controversial.
Objective To evaluate the effect of an SBT consisting of 30 minutes of pressure support ventilation (an approach that is less demanding for patients) vs an SBT consisting of 2 hours of T-piece ventilation (an approach that is more demanding for patients) on rates of successful extubation.
Design, Setting, and Participants Randomized clinical trial conducted from January 2016 to April 2017 among 1153 adults deemed ready for weaning after at least 24 hours of mechanical ventilation at 18 intensive care units in Spain. Follow-up ended in July 2017.
Interventions Patients were randomized to undergo a 2-hour T-piece SBT (n = 578) or a 30-minute SBT with 8-cm H2O pressure support ventilation (n = 557).
Main Outcome and Measures The primary outcome was successful extubation (remaining free of mechanical ventilation 72 hours after first SBT). Secondary outcomes were reintubation among patients extubated after SBT; intensive care unit and hospital lengths of stay; and hospital and 90-day mortality.
Results Among 1153 patients who were randomized (mean age, 62.2 [SD, 15.7] years; 428 [37.1%] women), 1018 (88.3%) completed the trial. Successful extubation occurred in 473 patients (82.3%) in the pressure support ventilation group and 428 patients (74.0%) in the T-piece group (difference, 8.2%; 95% CI, 3.4%-13.0%; P = .001). Among secondary outcomes, for the pressure support ventilation group vs the T-piece group, respectively, reintubation was 11.1% vs 11.9% (difference, −0.8%; 95% CI, −4.8% to 3.1%; P = .63), median intensive care unit length of stay was 9 days vs 10 days (mean difference, −0.3 days; 95% CI, −1.7 to 1.1 days; P = .69), median hospital length of stay was 24 days vs 24 days (mean difference, 1.3 days; 95% CI, −2.2 to 4.9 days; P = .45), hospital mortality was 10.4% vs 14.9% (difference, −4.4%; 95% CI, −8.3% to −0.6%; P = .02), and 90-day mortality was 13.2% vs 17.3% (difference, −4.1% [95% CI, −8.2% to 0.01%; P = .04]; hazard ratio, 0.74 [95% CI, 0.55-0.99]).
Conclusions and Relevance Among patients receiving mechanical ventilation, a spontaneous breathing trial consisting of 30 minutes of pressure support ventilation, compared with 2 hours of T-piece ventilation, led to significantly higher rates of successful extubation. These findings support the use of a shorter, less demanding ventilation strategy for spontaneous breathing trials.
Double AAP après revascularisation coronaire : OK 1 mois versus 1 an ?
Watanabe et al. JAMA 2019;321(24):2414-2427
doi :
Importance Very short mandatory dual antiplatelet therapy (DAPT) after percutaneous coronary intervention (PCI) with a drug-eluting stent may be an attractive option.
Objective To test the hypothesis of noninferiority of 1 month of DAPT compared with standard 12 months of DAPT for a composite end point of cardiovascular and bleeding events.
Design, Setting, and Participants Multicenter, open-label, randomized clinical trial enrolling 3045 patients who underwent PCI at 90 hospitals in Japan from December 2015 through December 2017. Final 1-year clinical follow-up was completed in January 2019.
Interventions Patients were randomized either to 1 month of DAPT followed by clopidogrel monotherapy (n=1523) or to 12 months of DAPT with aspirin and clopidogrel (n=1522).
Main Outcomes and Measures The primary end point was a composite of cardiovascular death, myocardial infarction (MI), ischemic or hemorrhagic stroke, definite stent thrombosis, or major or minor bleeding at 12 months, with a relative noninferiority margin of 50%. The major secondary cardiovascular end point was a composite of cardiovascular death, MI, ischemic or hemorrhagic stroke, or definite stent thrombosis and the major secondary bleeding end point was major or minor bleeding.
Results Among 3045 patients randomized, 36 withdrew consent; of 3009 remaining, 2974 (99%) completed the trial. One-month DAPT was both noninferior and superior to 12-month DAPT for the primary end point, occurring in 2.36% with 1-month DAPT and 3.70% with 12-month DAPT (absolute difference, −1.34% [95% CI, −2.57% to −0.11%]; hazard ratio [HR], 0.64 [95% CI, 0.42-0.98]), meeting criteria for noninferiority (P < .001) and for superiority (P = .04). The major secondary cardiovascular end point occurred in 1.96% with 1-month DAPT and 2.51% with 12-month DAPT (absolute difference, −0.55% [95% CI, −1.62% to 0.52%]; HR, 0.79 [95% CI, 0.49-1.29]), meeting criteria for noninferiority (P = .005) but not for superiority (P = .34). The major secondary bleeding end point occurred in 0.41% with 1-month DAPT and 1.54% with 12-month DAPT (absolute difference, −1.13% [95% CI, −1.84% to −0.42%]; HR, 0.26 [95% CI, 0.11-0.64]; P = .004 for superiority).
Conclusions and Relevance Among patients undergoing PCI, 1 month of DAPT followed by clopidogrel monotherapy, compared with 12 months of DAPT with aspirin and clopidogrel, resulted in a significantly lower rate of a composite of cardiovascular and bleeding events, meeting criteria for both noninferiority and superiority. These findings suggest that a shorter duration of DAPT may provide benefit, although given study limitations, additional research is needed in other populations.
Double AAP après revascularisation coronaire : OK 3 mois versus 1 an ?
Hahn et al. JAMA 2019;321(24):2428-2437
Importance Data on P2Y12 inhibitor monotherapy after short-duration dual antiplatelet therapy (DAPT) in patients undergoing percutaneous coronary intervention are limited.
Objective To determine whether P2Y12 inhibitor monotherapy after 3 months of DAPT is noninferior to 12 months of DAPT in patients undergoing PCI.
Design, Setting, and Participants The SMART-CHOICE trial was an open-label, noninferiority, randomized study that was conducted in 33 hospitals in Korea and included 2993 patients undergoing PCI with drug-eluting stents. Enrollment began March 18, 2014, and follow-up was completed July 19, 2018.
Interventions Patients were randomly assigned to receive aspirin plus a P2Y12 inhibitor for 3 months and thereafter P2Y12 inhibitor alone (n = 1495) or DAPT for 12 months (n = 1498).
Main Outcomes and Measures The primary end point was major adverse cardiac and cerebrovascular events (a composite of all-cause death, myocardial infarction, or stroke) at 12 months after the index procedure. Secondary end points included the components of the primary end point and bleeding defined as Bleeding Academic Research Consortium type 2 to 5. The noninferiority margin was 1.8%.
Results Among 2993 patients who were randomized (mean age, 64 years; 795 women [26.6%]), 2912 (97.3%) completed the trial. Adherence to the study protocol was 79.3% of the P2Y12 inhibitor monotherapy group and 95.2% of the DAPT group. At 12 months, major adverse cardiac and cerebrovascular events occurred in 42 patients in the P2Y12 inhibitor monotherapy group and in 36 patients in the DAPT group (2.9% vs 2.5%; difference, 0.4% [1-sided 95% CI, –∞% to 1.3%]; P = .007 for noninferiority). There were no significant differences in all-cause death (21 [1.4%] vs 18 [1.2%]; hazard ratio [HR], 1.18; 95% CI, 0.63-2.21; P = .61), myocardial infarction (11 [0.8%] vs 17 [1.2%]; HR, 0.66; 95% CI, 0.31-1.40; P = .28), or stroke (11 [0.8%] vs 5 [0.3%]; HR, 2.23; 95% CI, 0.78-6.43; P = .14) between the 2 groups. The rate of bleeding was significantly lower in the P2Y12 inhibitor monotherapy group than in the DAPT group (2.0% vs 3.4%; HR, 0.58; 95% CI, 0.36-0.92; P = .02).
Conclusions and Relevance Among patients undergoing percutaneous coronary intervention, P2Y12 inhibitor monotherapy after 3 months of DAPT compared with prolonged DAPT resulted in noninferior rates of major adverse cardiac and cerebrovascular events. Because of limitations in the study population and adherence, further research is needed in other populations.
Nouveau score de mortalité à long terme dans le sepsis ?
Shankar-Hari et al. JAMA Netw Open 2019;2(5):e194900
Atention à ne pas ultrafiltrer trop vite les patients en réa sous CVVHDF ?
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2735468
Importance Net ultrafiltration (NUF) is frequently used to treat fluid overload among critically ill patients, but whether the rate of NUF affects outcomes is unclear.
Objective To examine the association of NUF with survival among critically ill patients with acute kidney injury being treated with continuous venovenous hemodiafiltration.
Design, Setting, and Participants The Randomized Evaluation of Normal vs Augmented Level (RENAL) of Renal Replacement Therapy trial was conducted between December 30, 2005, and November 28, 2008, at 35 intensive care units in Australia and New Zealand among critically ill adults with acute kidney injury who were being treated with continuous venovenous hemodiafiltration. This secondary analysis began in May 2018 and concluded in January 2019.
Exposures Net ultrafiltration rate, defined as the volume of fluid removed per hour adjusted for patient body weight.
Main Outcomes and Measures Risk-adjusted 90-day survival.
Results Of 1434 patients, the median (interquartile range) age was 67.3 (56.9-76.3) years; 924 participants (64.4%) were male; median (interquartile range) Acute Physiology and Chronic Health Evaluation III score was 100 (84-118); and 634 patients (44.2%) died. Using tertiles, 3 groups were defined: high, NUF rate greater than 1.75 mL/kg/h; middle, NUF rate from 1.01 to 1.75 mL/kg/h; and low, NUF rate less than 1.01 mL/kg/h. The high-tertile group compared with the low-tertile group was not associated with death from day 0 to 6. However, death occurred in 51 patients (14.7%) in the high-tertile group vs 30 patients (8.6%) in the low-tertile group from day 7 to 12 (adjusted hazard ratio [aHR], 1.51; 95% CI, 1.13-2.02); 45 patients (15.3%) in the high-tertile group vs 25 patients (7.9%) in the low-tertile group from day 13 to 26 (aHR, 1.52; 95% CI, 1.11-2.07); and 48 patients (19.2%) in the high-tertile group vs 29 patients (9.9%) in the low-tertile group from day 27 to 90 (aHR, 1.66; 95% CI, 1.16-2.39). Every 0.5-mL/kg/h increase in NUF rate was associated with increased mortality (3-6 days: aHR, 1.05; 95% CI, 1.00-1.11; 7-12 days: aHR, 1.08; 95% CI, 1.02-1.15; 13-26 days: aHR, 1.11; 95% CI, 1.04-1.18; 27-90 days: aHR, 1.13; 95% CI, 1.05-1.22). Using longitudinal analyses, increase in NUF rate was associated with lower survival (β = .056; P < .001). Hypophosphatemia was more frequent among patients in the high-tertile group compared with patients in the middle-tertile group and patients in the low-tertile group (high: 308 of 477 patients at risk [64.6%]; middle: 293 of 472 patients at risk [62.1%]; low: 247 of 466 patients at risk [53.0%]; P < .001). Cardiac arrhythmias requiring treatment occurred among all groups: high, 176 patients (36.8%); middle: 175 patients (36.5%); and low: 147 patients (30.8%) (P = .08).
Conclusions and Relevance Among critically ill patients, NUF rates greater than 1.75 mL/kg/h compared with NUF rates less than 1.01 mL/kg/h were associated with lower survival. Residual confounding may be present from unmeasured risk factors, and randomized clinical trials are required to confirm these findings.
Impact de l’utilisation de l’ETT dans la prise en charge d’IDM ?
Pack et al.,
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2735988
Importance Guidelines recommend that patients with acute myocardial infarction (AMI) undergo echocardiography for assessment of cardiac structure and ejection fraction, but little is known about the association between echocardiography as used in routine clinical management of AMI and patient outcomes.
Objective To examine the association between risk-standardized hospital rates of transthoracic echocardiography and outcomes.
Design, Setting, and Participants This retrospective cohort study of data from 397 US hospitals that contributed to the Premier Healthcare Informatics inpatient database from January 1, 2014, to December 31, 2014, used International Classification of Diseases, Ninth Revision (ICD-9) codes to identify 98 999 hospital admissions for patients with AMI. Data were analyzed between October 2017 and January 2019.
Exposures Rates of transthoracic echocardiography.
Main Outcomes and Measures Inpatient mortality, length of stay, total inpatient costs, and 3-month readmission rate.
Results Among the 397 hospitals with more than 25 admissions for AMI in 2014, a total of 98 999 hospital admissions for AMI were identified for analysis (38.2% women; mean [SD] age, 66.5 [13.6] years), of which 69 652 (70.4%) had at least 1 transthoracic echocardiogram performed. The median (IQR) hospital risk-standardized rate of echocardiography was 72.5% (62.6%-79.1%). In models that adjusted for hospital and patient characteristics, no difference was found in inpatient mortality (odds ratio [OR], 1.02; 95% CI, 0.88-1.19) or 3-month readmission (OR, 1.01; 95% CI, 0.93-1.10) between the highest and lowest quartiles of echocardiography use (median risk-standardized echocardiography use rates of 83% vs 54%, respectively). However, hospitals with the highest rates of echocardiography had modestly longer mean lengths of stay (0.23 days; 95% CI, 0.04-0.41; P = .01) and higher mean costs ($3164; 95% CI, $1843-$4485; P < .001) per admission compared with hospitals in the lowest quartile of use. Multiple sensitivity analyses yielded similar results.
Conclusions and Relevance In patients with AMI, hospitals in the quartile with the highest rates of echocardiography showed greater hospital costs and length of stay but few differences in clinical outcomes compared with hospitals in the quartile with the lowest rates of echocardiography. These findings suggest that more selective use of echocardiography might be used without adversely affecting clinical outcomes, particularly in hospitals with high rates of echocardiography use.
Choc septique = Noradrénaline précoce ?
Rationale: Recent retrospective evidence suggests the efficacy of early norepinephrine administration during resuscitation; however, prospective data to support this assertion are scarce.
Objectives: To conduct a phase II trial evaluating the hypothesis that early low-dose norepinephrine in adults with sepsis with hypotension increases shock control by 6 hours compared with standard care.
Methods: This single-center, randomized, double-blind, placebo-controlled clinical trial was conducted at Siriraj Hospital, Bangkok, Thailand. The study enrolled 310 adults diagnosed with sepsis with hypotension. The patients were randomly divided into two groups: early norepinephrine (n = 155) and standard treatment (n = 155). The primary outcome was shock control rate (defined as achievement of mean arterial blood pressure ≥65 mm Hg, with urine flow ≥0.5 ml/kg/h for 2 consecutive hours, or decreased serum lactate ≥10% from baseline) by 6 hours after diagnosis.
Measurements and Main Results: The patients in both groups were well matched in background characteristics and disease severity. Median time from emergency room arrival to norepinephrine administration was significantly shorter in the early norepinephrine group (93 vs. 192 min; P < 0.001). Shock control rate by 6 hours was significantly higher in the early norepinephrine group (118/155 [76.1%] vs. 75/155 [48.4%]; P < 0.001). The 28-day mortality was not different between groups: 24/155 (15.5%) in the early norepinephrine group versus 34/155 (21.9%) in the standard treatment group (P = 0.15). The early norepinephrine group was associated with lower incidences of cardiogenic pulmonary edema (22/155 [14.4%] vs. 43/155 [27.7%]; P = 0.004) and new-onset arrhythmia (17/155 [11%] vs. 31/155 [20%]; P = 0.03).
Conclusions: Early norepinephrine was significantly associated with increased shock control by 6 hours. Further studies are needed before this approach is introduced in clinical resuscitation practice.
Impact des paramètres de ventilation chez le spatients sous ECMO
Schmidt et al. Am J Respir Crit Care Med 2019;epublished May 30th
https://doi.org/10.1164/rccm.201806-1094OC
Objectives: To report current practices regarding mechanical ventilation in patients treated with extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS) and their association with 6-month outcomes.
Methods: International, multi-center, prospective cohort study of patients undergoing ECMO for ARDS during a one-year period in 23 international intensive care units (ICUs).
Measurements and Main Results: We collected demographics, daily pre- and per-ECMO mechanical ventilation settings and use of adjunctive therapies, ICU- and 6-month–outcome data for 350 patients (median ± standard deviation pre-ECMO PaO2/FiO2 71±34 mmHg). Pre-ECMO use of prone positioning and neuromuscular blockers were 26% and 62%, respectively. Tidal volume (6.4±2.0 vs 3.7±2.0 ml/kg), plateau pressure (32±7 vs 24±7cmH2O), driving pressure (20±7 vs. 14±4 cmH2O), respiratory rate (26±8 vs 14±6 breaths/min) and mechanical power (26.1±12.7 vs. 6.6±4.8 J/min) were markedly reduced after ECMO initiation. Six-month survival was 61%. No association was found between ventilator settings during the first 2 days of ECMO and survival in multivariable analysis. A time-varying Cox model retained older age, higher fluid balance, higher lactate, and more need for renal replacement therapy along the ECMO course as being independently associated with 6-month mortality. A higher tidal volume and lower driving pressure (likely markers of static compliance improvement) across the ECMO course were also associated with better outcomes.
Conclusion: Ultra-protective lung ventilation on ECMO was largely adopted across medium to high case-volume ECMO centers. In contrast with previous observations, mechanical ventilation settings during ECMO did not impact patients’ prognosis in this context.
La dyspnée, sous diagnostiquée et sous traitée ?
Underdetection and Undertreatment of Dyspnea in Critically Ill Patients.
Gentzler et al. Am J Respir Crit Care Med 2019;199(11):1377–1384
https://doi.org/10.1164/rccm.201805-0996OC
Rationale: Dyspnea is a common and distressing physical symptom among patients in the ICU and may be underdetected and undertreated.
Objectives: To determine the frequency of dyspnea relative to pain, the accuracy of nurses and personal caregiver dyspnea ratings relative to patient-reported dyspnea, and the relationship between nurse-detected dyspnea and treatment.
Methods: This was an observational study of patients (n = 138) hospitalized in a medical ICU (MICU). Nurses and patients’ personal caregivers at the bedside reported on their perception of patients’ symptoms.
Measurements and Main Results: Dyspnea was assessed by patients, caregivers, and nurses with a numerical rating scale. Across all three raters, the frequency of moderate to severe dyspnea was similar or greater than that of pain (P < 0.05 for caregiver and nurse ratings). Personal caregivers’ ratings of dyspnea had substantial agreement with patient ratings (κ = 0.65, P < 0.001), but nurses’ ratings were not significantly related to patient ratings (κ = 0.19, P = 0.39). Nurse detection of moderate to severe pain was significantly associated with opioid treatment (odds ratio, 2.70; 95% confidence interval, 1.10–6.60; P = 0.03); however, nurse detection of moderate to severe dyspnea was not significantly associated with any assessed treatment.
Conclusions: Dyspnea was reported at least as frequently as pain among the sampled MICU patients. Personal caregivers had good agreement with patient reports of moderate to severe dyspnea. However, even when detected by nurses, dyspnea appeared to be undertreated. These findings suggest the need for improved detection and treatment of dyspnea in the MICU.
ROX = Indice (SpO2/FiO2) mieux que la FR pour prédire l’échec d’Optiflow ?
An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy.
Roca et al. Am J Respir Crit Care Med 2019;199(11):1368–1376
https://doi.org/10.1164/rccm.201803-0589OC
Rationale: One important concern during high-flow nasal cannula (HFNC) therapy in patients with acute hypoxemic respiratory failure is to not delay intubation.
Objectives: To validate the diagnostic accuracy of an index (termed ROX and defined as the ratio of oxygen saturation as measured by pulse oximetry/FiO2 to respiratory rate) for determining HFNC outcome (need or not for intubation).
Methods: This was a 2-year multicenter prospective observational cohort study including patients with pneumonia treated with HFNC. Identification was through Cox proportional hazards modeling of ROX association with HFNC outcome. The most specific cutoff of the ROX index to predict HFNC failure and success was assessed.
Measurements and Main Results: Among the 191 patients treated with HFNC in the validation cohort, 68 (35.6%) required intubation. The prediction accuracy of the ROX index increased over time (area under the receiver operating characteristic curve: 2 h, 0.679; 6 h, 0.703; 12 h, 0.759). ROX greater than or equal to 4.88 measured at 2 (hazard ratio, 0.434; 95% confidence interval, 0.264–0.715; P = 0.001), 6 (hazard ratio, 0.304; 95% confidence interval, 0.182–0.509; P < 0.001), or 12 hours (hazard ratio, 0.291; 95% confidence interval, 0.161–0.524; P < 0.001) after HFNC initiation was consistently associated with a lower risk for intubation. A ROX less than 2.85, less than 3.47, and less than 3.85 at 2, 6, and 12 hours of HFNC initiation, respectively, were predictors of HFNC failure. Patients who failed presented a lower increase in the values of the ROX index over the 12 hours. Among components of the index, oxygen saturation as measured by pulse oximetry/FiO2 had a greater weight than respiratory rate.
Conclusions: In patients with pneumonia with acute respiratory failure treated with HFNC, ROX is an index that can help identify those patients with low and those with high risk for intubation.
Outcomes chez les patients ayant eu une ventilation mécanique prolongée
Long-Term Outcome after Prolonged Mechanical Ventilation. A Long-Term Acute-Care Hospital Study.
Jubran et al. Am J Respir Crit Care Med 2019;199(12):1508–1516
https://doi.org/10.1164/rccm.201806-1131OC
Rationale: Patients managed at a long-term acute-care hospital (LTACH) for weaning from prolonged mechanical ventilation are at risk for profound muscle weakness and disability.
Objectives: To investigate effects of prolonged ventilation on survival, muscle function, and its impact on quality of life at 6 and 12 months after LTACH discharge.
Methods: This was a prospective, longitudinal study conducted in 315 patients being weaned from prolonged ventilation at an LTACH.
Measurements and Main Results: At discharge, 53.7% of patients were detached from the ventilator and 1-year survival was 66.9%. On enrollment, maximum inspiratory pressure (Pimax) was 41.3 (95% confidence interval, 39.4–43.2) cm H2O (53.1% predicted), whereas handgrip strength was 16.4 (95% confidence interval, 14.4–18.7) kPa (21.5% predicted). At discharge, Pimax did not change, whereas handgrip strength increased by 34.8% (P < 0.001). Between discharge and 6 months, handgrip strength increased 6.2 times more than did Pimax. Between discharge and 6 months, Katz activities-of-daily-living summary score improved by 64.4%; improvement in Katz summary score was related to improvement in handgrip strength (r = −0.51; P < 0.001). By 12 months, physical summary score and mental summary score of 36-item Short-Form Survey returned to preillness values. When asked, 84.7% of survivors indicated willingness to undergo mechanical ventilation again.
Conclusions: Among patients receiving prolonged mechanical ventilation at an LTACH, 53.7% were detached from the ventilator at discharge and 1-year survival was 66.9%. Respiratory strength was well maintained, whereas peripheral strength was severely impaired throughout hospitalization. Six months after discharge, improvement in muscle function enabled patients to perform daily activities, and 84.7% indicated willingness to undergo mechanical ventilation again.
Stop aux antigénuries Légionnelle et Pneumocoque systématiques ?
https://academic.oup.com/cid/article-abstract/68/12/2026/5108546?redirectedFrom=fulltext
Adult, community-acquired pneumonia (CAP) guidelines from the Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) include indications for urinary antigen tests (UATs) for Streptococcus pneumoniae (SP) and Legionella pneumophila (LP). These recommendations were based on expert opinions and have not been rigorously evaluated.
We used data from a multicenter, prospective, surveillance study of adults hospitalized with CAP to evaluate the sensitivity and specificity of the IDSA/ATS UAT indications for identifying patients who test positive. SP and LP UATs were completed on all included patients. Separate analyses were completed for SP and LP, using 2-by-2 contingency tables, comparing the IDSA/ATS indications (UAT recommended vs not recommended) and UAT results (positive vs negative). Additionally, logistic regression was used to evaluate the association of each individual criterion in the IDSA/ATS indications with positive UAT results.
Among 1941 patients, UATs were positive for SP in 81 (4.2%) and for LP in 32 (1.6%). IDSA/ATS indications had 61% sensitivity (95% confidence interval [CI] 49–71%) and 39% specificity (95% CI 37–41%) for SP, and 63% sensitivity (95% CI 44–79%) and 35% specificity (95% CI 33–37%) for LP. No clinical characteristics were strongly associated with positive SP UATs, while features associated with positive LP UATs were hyponatremia, fever, diarrhea, and recent travel.
Recommended indications for SP and LP urinary antigen testing in the IDSA/ATS CAP guidelines have poor sensitivity and specificity for identifying patients with positive tests; future CAP guidelines should consider other strategies for determining which patients should undergo urinary antigen testing.
VRS plus grave chez la personne âgée que la grippe ?
Respiratory syncytial virus (RSV) is an important cause of serious respiratory illness in older adults. Comparison of RSV and influenza infection in hospitalized older adults may increase awareness of adult RSV disease burden.
Hospitalized adults aged ≥60 years who tested positive for RSV or influenza between 1 January 2011 and 30 June 2015 were identified from Kaiser Permanente Southern California electronic medical records. Baseline characteristics, comorbidities, utilization, and outcomes were compared.
The study included 645 RSV- and 1878 influenza-infected hospitalized adults. Patients with RSV were older than those with influenza (mean, 78.5 vs 77.4 years; P = .035) and more likely to have congestive heart failure (35.3% vs 24.5%; P < .001) and chronic obstructive pulmonary disease (COPD) (29.8% vs 24.3%; P = .006) at baseline. In adjusted analyses, RSV infection was associated with greater odds of length of stay ≥7 days (odds ratio [OR] = 1.5; 95% confidence interval [CI], 1.2–1.8; P < .001); pneumonia (OR = 2.7; 95% CI, 2.2–3.2; P < .001); intensive care unit admission (OR = 1.3; 95% CI, 1.0–1.7; P = .023); exacerbation of COPD (OR = 1.7; 95% CI, 1.3–2.4; P = .001); and greater mortality within 1 year of admission (OR = 1.3; 95% CI, 1.0–1.6; P = .019).
RSV infection may result in greater morbidity and mortality among older hospitalized adults than influenza. Increased recognition of adult RSV disease burden will be important in the evaluation and use of new RSV vaccines and antivirals.
PBR chez le patient en réanimation : diagnostic et traitement
de Chambrun, et al., CCM, 2019
doi: 10.1097/CCM.0000000000003634
Objectives: Transvenous renal biopsy is an alternative way to obtain kidney samples from patients with bleeding risk factors (e.g., antiplatelet therapy and anticoagulation or coagulation disorders). This study was undertaken to determine the safety and diagnostic yield of transvenous renal biopsy of critically ill patients.
Design: Monocenter, retrospective, observational cohort study.
Setting: A 26-bed French tertiary ICU.
Patients: All patients undergoing in-ICU transvenous renal biopsy between January 2002 and February 2018.
Interventions: None.
Measurements and Main Results: Eighty patients (male/female sex ratio, 0.95; mean ± sd age, 47.3 ± 18.3 yr) were included. A histologic diagnosis was obtained for 77 patients (96.3%), with acute tubular necrosis being the most frequent: 23 (29.9%). A potentially treatable cause was found for 47 patients (58.7%). The numbers of patients with 0, 1, 2, or 3 factors (i.e., antiplatelet therapy, thrombopenia [< 150 G/L], and preventive or curative anticoagulation) at the time of the biopsy were, respectively: seven (8.8%), 37 (46.2%), 31 (38.7%), and five (6.3%). Four (5%) and two (2.5%) patients, respectively, had renal hematoma and macroscopic hematuria; none required any specific treatment. Six patients (7.5%) died in-ICU, and 90-day mortality was 8 of 80 (10%). No death was related to transvenous renal biopsy, and median biopsy-to-death interval was 38 days (interquartile range, 19.7–86 d).
Conclusions: Based on this cohort of ICU patients with acute kidney injury, transvenous renal biopsy was safe and obtained a high diagnostic yield for these selected critically ill patients, even in the presence of multiple bleeding risk factors.
Le retour du Pentho ?
PURPOSE: Propofol is commonly used with remifentanil for induction of general anesthesia (GA); however, it often leads to hypotension. Intraoperative hypotension is associated with postoperative adverse events. By contrast, thiopental has less negative inotropic effects on hemodynamics compared to propofol, which could be suitable to prevent hypotension during GA induction. In the present age-stratified, randomized, assessor-blinded study, using the ClearSight® system, we compared the hemodynamic effects of propofol and thiopental during GA induction under remifentanil infusion in non-cardiac surgery.
METHODS: Patients were divided into young (20-40 year), middle (41-70 year), and elderly (> 70 year) groups (n = 20, each group). General anesthesia was induced with remifentanil 0.3 μg/kg/min, followed by propofol (2.0, 1.5, and 1.2 mg/kg) or thiopental (5.0, 4.0, and 3.0 mg/kg) in the young, middle, and elderly groups, respectively. The primary outcome was the difference in the decrease in mean arterial blood pressure between patients receiving propofol and thiopental in each age group. The secondary outcomes included other hemodynamic parameters and minimal bispectral index values measured up to 10 min after tracheal intubation.
RESULTS: The decrease in mean arterial blood pressure was greater in patients receiving propofol than those receiving thiopental (- 45.4 vs – 26.6 mmHg and – 45.7 vs – 28.9 mmHg, P = 0.003 and 0.007, respectively), whereas no significant difference was observed in the young age group (P = 0.96).
CONCLUSIONS: Thiopental is a more suitable agent than propofol for avoiding hypotension during GA induction under remifentanil infusion in the middle and elderly patients.
Taux d’intubation au 1er coup : impact du sexe de l’opérateur ?
De la médecine traditionnelle chinoise pour avancer sur les pneumonies communautaires sévères ?
Objectives: To investigate whether XueBiJing injection improves clinical outcomes in critically ill patients with severe community-acquired pneumonia.
Design: Prospective, randomized, controlled study.
Setting: Thirty-three hospitals in China.
Patients: A total of 710 adults 18–75 years old with severe community-acquired pneumonia.
Interventions: Participants in the XueBiJing group received XueBiJing, 100 mL, q12 hours, and the control group received a visually indistinguishable placebo.
Measurements and Main Results: The primary outcome was 8-day improvement in the pneumonia severity index risk rating. Secondary outcomes were 28-day mortality rate, duration of mechanical ventilation and total duration of ICU stay. Improvement in the pneumonia severity index risk rating, from a previously defined endpoint, occurred in 203 (60.78%) participants receiving XueBiJing and in 158 (46.33%) participants receiving placebo (between-group difference [95% CI], 14.4% [6.9–21.8%]; p < 0.001). Fifty-three (15.87%) XueBiJing recipients and 84 (24.63%) placebo recipients (8.8% [2.4–15.2%]; p = 0.006) died within 28 days. XueBiJing administration also decreased the mechanical ventilation time and the total ICU stay duration. The median mechanical ventilation time was 11.0 versus 16.5 days for the XueBiJing and placebo groups, respectively (p = 0.012). The total duration of ICU stay was 12 days for XueBiJing recipients versus 16 days for placebo recipients (p = 0.004). A total of 256 patients experienced adverse events (119 [35.63%] vs 137 [40.18%] in the XueBiJing and placebo groups, respectively [p = 0.235]).
Conclusions: In critically ill patients with severe community-acquired pneumonia, XueBiJing injection led to a statistically significant improvement in the primary endpoint of the pneumonia severity index as well a significant improvement in the secondary clinical outcomes of mortality, duration of mechanical ventilation and duration of ICU stay.
Deep learning sur EEG pour prédire le pronostic neurologique post-ACR
Outcome Prediction in Postanoxic Coma With Deep Learning.
Tjepkema-Cloostermans et al. Crit Care Med 2019;epublished June 3rd
DOI: 10.1097/CCM.0000000000003854
Objectives:Visual assessment of the electroencephalogram by experienced clinical neurophysiologists allows reliable outcome prediction of approximately half of all comatose patients after cardiac arrest. Deep neural networks hold promise to achieve similar or even better performance, being more objective and consistent.
Design:Prospective cohort study.Setting:Medical ICU of five teaching hospitals in the Netherlands.
Patients:Eight-hundred ninety-five consecutive comatose patients after cardiac arrest.Interventions:None.
Measurements and Main Results:Continuous electroencephalogram was recorded during the first 3 days after cardiac arrest. Functional outcome at 6 months was classified as good (Cerebral Performance Category 1–2) or poor (Cerebral Performance Category 3–5). We trained a convolutional neural network, with a VGG architecture (introduced by the Oxford Visual Geometry Group), to predict neurologic outcome at 12 and 24 hours after cardiac arrest using electroencephalogram epochs and outcome labels as inputs. Output of the network was the probability of good outcome. Data from two hospitals were used for training and internal validation (n = 661). Eighty percent of these data was used for training and cross-validation, the remaining 20% for independent internal validation. Data from the other three hospitals were used for external validation (n = 234). Prediction of poor outcome was most accurate at 12 hours, with a sensitivity in the external validation set of 58% (95% CI, 51–65%) at false positive rate of 0% (CI, 0–7%). Good outcome could be predicted at 12 hours with a sensitivity of 48% (CI, 45–51%) at a false positive rate of 5% (CI, 0–15%) in the external validation set.
Conclusions:Deep learning of electroencephalogram signals outperforms any previously reported outcome predictor of coma after cardiac arrest, including visual electroencephalogram assessment by trained electroencephalogram experts. Our approach offers the potential for objective and real time, bedside insight in the neurologic prognosis of comatose patients after cardiac arrest.
L’insuffisance rénale aigue + SDRA = surmortalité
McNicholas et al. Crit Care Med 2019;epublished May 31st
DOI: 10.1097/CCM.0000000000003832
Objectives:To understand the impact of mild-moderate and severe acute kidney injury in patients with acute respiratory distress syndrome.
Design:Secondary analysis of the “Large Observational Study to Understand the Global Impact of Severe Acute Respiratory Failure”, an international prospective cohort study of patients with severe respiratory failure.Setting:Four-hundred fifty-nine ICUs from 50 countries across five continents.
Subjects:Patients with a glomerular filtration rate greater than 60 mL/min/1.73 m2 prior to admission who fulfilled criteria of acute respiratory distress syndrome on day 1 and day 2 of acute hypoxemic respiratory failure.Interventions:Patients were categorized based on worst serum creatinine or urine output into: 1) no acute kidney injury (serum creatinine < 132 µmol/L or urine output ≥ 0.5 mL/kg/hr), 2) mild-moderate acute kidney injury (serum creatinine 132–354 µmol/L or minimum urine output between 0.3 and 0.5mL/kg/hr), or 3) severe acute kidney injury (serum creatinine > 354 µmol/L or renal replacement therapy or minimum urine output < 0.3 mL/kg/hr).Measurements and Main
Results:The primary outcome was hospital mortality, whereas secondary outcomes included prevalence of acute kidney injury and characterization of acute respiratory distress syndrome risk factors and illness severity patterns, in patients with acute kidney injury versus no acute kidney injury. One-thousand nine-hundred seventy-four patients met inclusion criteria: 1,209 (61%) with no acute kidney injury, 468 (24%) with mild-moderate acute kidney injury, and 297 (15%) with severe acute kidney injury. The impact of acute kidney injury on the ventilatory management of patients with acute respiratory distress syndrome was relatively limited, with no differences in arterial CO2 tension or in tidal or minute ventilation between the groups. Hospital mortality increased from 31% in acute respiratory distress syndrome patients with no acute kidney injury to 50% in mild-moderate acute kidney injury (p ≤ 0.001 vs no acute kidney injury) and 58% in severe acute kidney injury (p ≤ 0.001 vs no acute kidney injury and mild-moderate acute kidney injury). In multivariate analyses, both mild-moderate (odds ratio, 1.61; 95% CI, 1.24–2.09; p < 0.001) and severe (odds ratio, 2.13; 95% CI, 1.55–2.94; p < 0.001) acute kidney injury were independently associated with mortality.
Conclusions:The development of acute kidney injury, even when mild-moderate in severity, is associated with a substantial increase in mortality in patients with acute respiratory distress syndrome.
La PEEP seule suffit à diminuer les atélectasies ?
Positive End-expiratory Pressure and Postoperative Atelectasis: A Randomized Controlled Trial.
Östberg et al. Anesthesiology 2019;epublished May 14th
DOI:10.1097/ALN.0000000000002764
BACKGROUND:
Various methods for protective ventilation are increasingly being recommended for patients undergoing general anesthesia. However, the importance of each individual component is still unclear. In particular, the perioperative use of positive end-expiratory pressure (PEEP) remains controversial. The authors tested the hypothesis that PEEP alone would be sufficient to limit atelectasis formation during nonabdominal surgery.
METHODS:
This was a randomized controlled evaluator-blinded study. Twenty-four healthy patients undergoing general anesthesia were randomized to receive either mechanical ventilation with PEEP 7 or 9 cm H2O depending on body mass index (n = 12) or zero PEEP (n = 12). No recruitment maneuvers were used. The primary outcome was atelectasis area as studied by computed tomography in a transverse scan near the diaphragm, at the end of surgery, before emergence. Oxygenation was evaluated by measuring blood gases and calculating the ratio of arterial oxygen partial pressure to inspired oxygen fraction (PaO2/FIO2 ratio).
RESULTS:
At the end of surgery, the median (range) atelectasis area, expressed as percentage of the total lung area, was 1.8 (0.3 to 9.9) in the PEEP group and 4.6 (1.0 to 10.2) in the zero PEEP group. The difference in medians was 2.8% (95% CI, 1.7 to 5.7%; P = 0.002). Oxygenation and carbon dioxide elimination were maintained in the PEEP group, but both deteriorated in the zero PEEP group.
CONCLUSIONS:
During nonabdominal surgery, adequate PEEP is sufficient to minimize atelectasis in healthy lungs and thereby maintain oxygenation. Thus, routine recruitment maneuvers seem unnecessary, and the authors suggest that they should only be utilized when clearly indicated.
Haldol prophylactique sur la qualité de vie à long terme chez les patients en réa à haut risque de Delirium ?
doi:10.1097/ALN.0000000000002812
Background: Delirium incidence in intensive care unit patients is high and associated with impaired long-term outcomes. The use of prophylactic haloperidol did not improve short-term outcome among critically ill adults at high risk of delirium. This study evaluated the effects of prophylactic haloperidol use on long-term quality of life in this group of patients and explored which factors are associated with change in quality of life.
Methods: A preplanned secondary analysis of long-term outcomes of the pRophylactic haloperidol usE for DeliriUm in iCu patients at high risk for dElirium (REDUCE) study was conducted. In this multicenter randomized clinical trial, nondelirious intensive care unit patients were assigned to prophylactic haloperidol (1 or 2 mg) or placebo (0.9% sodium chloride). In all groups, patients finally received study medication for median duration of 3 days [interquartile range, 2 to 6] until onset of delirium or until intensive care unit discharge. Long-term outcomes were assessed using the Short Form-12 questionnaire at intensive care unit admission (baseline) and after 1 and 6 months. Quality of life was summarized in the physical component summary and mental component summary scores. Differences between the haloperidol and placebo group and factors associated with changes in quality of life were analyzed.
Results: Of 1,789 study patients, 1,245 intensive care unit patients were approached, of which 887 (71%) responded. Long-term quality of life did not differ between the haloperidol and placebo group (physical component summary mean score of 39 ± 11 and 39 ± 11, respectively, and P = 0.350; and mental component summary score of 50 ± 10 and 51 ± 10, respectively, and P = 0.678). Age, medical and trauma admission, quality of life score at baseline, risk for delirium (PRE-DELIRIC) score, and the number of sedation-induced coma days were significantly associated with a decline in long-term quality of life.
Conclusions: Prophylactic haloperidol use does not affect long-term quality of life in critically ill patients at high risk for delirium. Several factors, including the modifiable factor number of sedation-induced coma days, are associated with decline in long-term outcomes.
ACR extra-hospitalier = Masser et seulement masser !
Riva et al. Circulation 2019;139:2600–2609
https://doi.org/10.1161/CIRCULATIONAHA.118.038179
Background:
In out-of-hospital cardiac arrest, chest compression–only cardiopulmonary resuscitation (CO-CPR) has emerged as an alternative to standard CPR (S-CPR), using both chest compressions and rescue breaths. Since 2010, CPR guidelines recommend CO-CPR for both untrained bystanders and trained bystanders unwilling to perform rescue breaths. The aim of this study was to describe changes in the rate and type of CPR performed before the arrival of emergency medical services (EMS) during 3 consecutive guideline periods in correlation to 30-day survival.
Methods:
All bystander-witnessed out-of-hospital cardiac arrests reported to the Swedish register for cardiopulmonary resuscitation in 2000 to 2017 were included. Nonwitnessed, EMS-witnessed, and rescue breath–only CPR cases were excluded. Patients were categorized as receivers of no CPR (NO-CPR), S-CPR, or CO-CPR before EMS arrival. Guideline periods 2000 to 2005, 2006 to 2010, and 2011 to 2017 were used for comparisons over time. The primary outcome was 30-day survival.
Results:
A total of 30 445 patients were included. The proportions of patients receiving CPR before EMS arrival changed from 40.8% in the first time period to 58.8% in the second period, and to 68.2% in the last period. S-CPR changed from 35.4% to 44.8% to 38.1%, and CO-CPR changed from 5.4% to 14.0% to 30.1%, respectively. Thirty-day survival changed from 3.9% to 6.0% to 7.1% in the NO-CPR group, from 9.4% to 12.5% to 16.2% in the S-CPR group, and from 8.0% to 11.5% to 14.3% in the CO-CPR group. For all time periods combined, the adjusted odds ratio for 30-day survival was 2.6 (95% CI, 2.4–2.9) for S-CPR and 2.0 (95% CI, 1.8–2.3) for CO-CPR, in comparison with NO-CPR. S-CPR was superior to CO-CPR (adjusted odds ratio, 1.2; 95% CI, 1.1–1.4).
Conclusions:
In this nationwide study of out-of-hospital cardiac arrest during 3 periods of different CPR guidelines, there was an almost a 2-fold higher rate of CPR before EMS arrival and a concomitant 6-fold higher rate of CO-CPR over time. Any type of CPR was associated with doubled survival rates in comparison with NO-CPR. These findings support continuous endorsement of CO-CPR as an option in future CPR guidelines because it is associated with higher CPR rates and overall survival in out-of-hospital cardiac arrest.
Doppler Transcranien pour le pronostic précoce post-ACR extrahospitalier ?
Aim
To assess the neurological prognosis of comatose survivors of cardiac arrest by early transcranial Doppler sonography (TCD).
Methods
This was a prospective study performed between May 2016 and October 2017 in a medical intensive care unit (ICU) and a cardiac ICU of a university teaching hospital.
All patients older than 18 years who were successfully resuscitated from an out-of-hospital cardiac arrest (OHCA) with persistent coma after the return of spontaneous circulation (ROSC) were eligible. We excluded patients for whom OHCA was associated with traumatic brain injury, no possibility of TCD measurements, or who were dead before establishing the neurological prognosis.
We measured the pulsatility index (PI) and diastolic flow velocity (DFV) of the right and left middle cerebral arteries within 12 h after ICU admission. The lowest DFV and highest PI values were used for the statistical analysis. The neurological outcome at hospital discharge was evaluated by the cerebral performance category.
Results
Forty-two patients were included in the final analysis: 15 had good and 27 poor neurological outcomes. The PI was higher in the poor outcome (1.49 vs. 1.12, p = 0.01) than good outcome group and the DFV was lower in the poor outcome group (17.3 cm s−1 vs. 26.0 cm s−1; p = 0.01).
Conclusion
Data provided by early TCD after ROSC are associated with neurological outcome. The use of TCD could help guide interventions to improve cerebral perfusion after ROSC in patients resuscitated from OHCA.
Pression intracrânienne normale mais troubles de compliance cérébrale en cas de lésions ischémiques post-ACR ?
Intracranial pressure and compliance in hypoxic ischemic brain injury patients after cardiac arrest.
Sekhon et al. Resuscitation 2019;epublished June 8th
DOI: https://doi.org/10.1016/j.resuscitation.2019.05.036
Introduction
In hypoxic ischemic brain injury (HIBI), increased intracranial pressure (ICP) can ensue from cerebral edema stemming from cytotoxic and vasogenic mechanisms. Downstream sequelae of restricted cerebral blood flow lead to neurologic braindeath. There is limited data characterizing the temporal trends and patterns of ICP and compliance in human HIBI patients.
Methods
Patients underwent invasive ICP monitoring with a parenchymal probe (Camino) and were managed with a tier-based management algorithm for elevated ICP. Data pertaining to mean arterial pressure (MAP), ICP, brain tissue oxygenation (PbtO2), end tidal carbon dioxide (ETCO2), core body temperature and RAP (moving correlation coefficient between mean ICP and its mean pulse amplitude) as a measure of intracranial compliance were recorded in the ICM + software. Data pertaining to ICP lowering interventions was also collected.
Results
Ten patients were included with a median age of 47 (range 20–71) and seven were male (7/10). The mean ICP was 14 mmHg (SD 11) and time of ICP> 20 mmHg was 22% (range 0–100). The mean MAP, ETCO2 and temperature were 89 mmHg (SD 13), 31 mmHg (SD 7), 35.7 °C (SD 0.9), respectively. The mean RAP was 0.58 (SD 0.34) and time of RAP > 0.4 was 78% (range 57–97). There were no significant relationships between ETCO2 and temperature with ICP.
Conclusions
In our cohort, HIBI was characterized by normal ICP but with limited intracranial compliance. However, significant in between patient heterogeneity exists with respect to temporal patterns of intracranial pressure — volume relationships in HIBI.
Des soins intensifs pour les patients avec un infarctus
https://www.bmj.com/content/bmj/365/bmj.l1927.full.pdf
Valley et al. BMJ 2019;365:l1927
Oligurie per-op : associée à l’IRA mais mauvaise prédiction
Myles et al. Br J Anaesth 2019;122(6):726–733
Background
The association between intraoperative oliguria during major abdominal surgery and the subsequent development of postoperative acute kidney injury (AKI) remains poorly defined. We hypothesised that, in such patients, intraoperative oliguria would be an independent predictor of subsequent AKI.
Methods
We performed a post hoc analysis of data from the Restrictive versus Liberal Fluid Therapy in Major Abdominal Surgery (RELIEF) trial of conservative vs liberal fluid therapy during and after major abdominal surgery. We used χ2, logistic regression, and fractional polynomials to study the association between intraoperative oliguria defined as a urinary output <0.5 ml kg−1 h−1 and the development of postoperative AKI defined by the Kidney Disease Improving Global Outcomes consensus criteria.
Results
We included 2444 of 2983 patients from the RELIEF trial in this study. A total of 889 patients (36%) met oliguric criteria intraoperatively. Oliguria occurred in 35% of those without AKI, and 44%, 48%, and 45% of those who developed postoperative AKI Stages 1–3, respectively (P<0.001 for trend). Intraoperative oliguria was associated with an increased risk of AKI, risk ratio: 1.38 (95% confidence interval: 1.14–1.44; P<0.001), but greater intensity of oliguria (urine output <0.3 ml kg−1 h−1) did not increase this risk further. Most patients with oliguria did not develop AKI; the positive predictive value of oliguria was 25.5%, and the negative predictive value was 81.6%.
Conclusions
Intraoperative oliguria, defined as urine output <0.5 ml kg−1 h−1, was relatively common and was associated with postoperative AKI. However, the predictive utility of oliguria for AKI was low, whilst its absence had a good predictive value for an AKI-free postoperative course.
Surtout pas de manoeuvre de recrutement pour les patients en SDRA choqués sur une pneumonie ? Résultats de machine learning
Zampieri et al. Br J Anaesth 2019;123(1):88–95
Background
Despite a robust physiological rationale, recruitment manoeuvres with PEEP titration were associated with harm in the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART). We sought to investigate the potential heterogeneity in treatment effects in patients enrolled in the ART, using a machine learning approach.
Methods
The primary outcome was hospital mortality. Patients were clustered using baseline clinical and physiological data using the k-means for mixed large data method. The heterogeneity in treatment effect between clusters was investigated using Bayesian methods. We further investigated whether baseline driving pressure could modulate the association between treatment arm, cluster, and mortality.
Results
Data from all 1010 patients enrolled in the ART were analysed. Partitioning suggested that three clusters were present in the ART population. The largest cluster (Cluster 1) was characterised by patients with pneumonia and requiring vasopressor support. Recruitment manoeuvres with PEEP titration were associated with higher mortality in Cluster 1 (probability of harm of >98%), but this association was absent in Clusters 2 and 3 (probability of harm of 45% and 68%, respectively). Higher baseline driving pressure was associated with a progressive reduction in the association between alveolar recruitment with PEEP titration and mortality.
Conclusions
Recruitment manoeuvre with PEEP titration may be harmful in acute respiratory distress syndrome (ARDS) patients with pneumonia or requiring vasopressor support. Driving pressure appears to modulate the association between the ART study intervention, aetiology of ARDS, and mortality. This machine learning approach may help tailor future RCTs.
Réactions d’hypersenbilité péri-opératoire
– Revue de ce qui se fait dans le Monde :
Mertes et al. Br J Anaesth 2019;123(1):e16–e28
-Recommendations internationales :
– Gestion type du patient « allergique à la pénicilline »
Méta-analyse : baisse de la mortalité en onco-réanimation sauf chez les patients allogreffés de moelle ?
Intérêt de l’ETO continue dans la gestion des états de choc en Réa ?
Purpose
Mortality in circulatory shock is high. Enhanced resolution of shock may improve outcomes. We aim to determine whether adding hemodynamic monitoring with continual transesophageal echocardiography (hTEE) to usual care accelerates resolution of hemodynamic instability.
Methods
550 patients with circulatory shock were randomly assigned to four groups stratified using hTEE (hTEE vs usual care) and assessment frequency (minimum every 4 h vs 8 h). Primary outcome was time to resolution of hemodynamic instability, analyzed as intention-to-treat (ITT) analysis at day 6 and in a predefined secondary analysis at days 3 and 28.
Results
Of 550 randomized patients, 271 with hTEE and 274 patients with usual care were eligible and included in the ITT analysis. Time to resolution of hemodynamic instability did not differ within the first 6 days [hTEE vs usual care adjusted sub-hazard ratio (SHR) 1.20, 95% confidence interval (CI) 0.98–1.46, p = 0.067]. Time to resolution of hemodynamic instability during the 72 h of hTEE monitoring was shorter in patients with TEE (hTEE vs usual care SHR 1.26, 95% CI 1.02–1.55, p = 0.034). Assessment frequency had no influence. Time to resolution of clinical signs of hypoperfusion, duration of organ support, length of stay and mortality in the intensive care unit and hospital, and mortality at 28 days did not differ between groups.
Conclusions
In critically ill patients with shock, hTEE monitoring or hemodynamic assessment frequency did not influence resolution of hemodynamic instability or mortality within the first 6 days.
Impact écologique de la DDS
Background
The long-term ecological effects on the emergence of antimicrobial resistance at the ICU level during selective decontamination of the digestive tract (SDD) are unknown. We determined the incidence of newly acquired antimicrobial resistance of aerobic gram-negative potentially pathogenic bacteria (AGNB) during SDD.
Methods
In a single-centre observational cohort study over a 21-year period, all consecutive patients, treated with or without SDD, admitted to the ICU were included. The antibiotic regime was unchanged over the study period. Incidence rates for ICU-acquired AGNB’s resistance for third-generation cephalosporins, colistin/polymyxin B, tobramycin/gentamicin or ciprofloxacin were calculated per year. Changes over time were tested by negative binomial regression in a generalized linear model.
Results
Eighty-six percent of 14,015 patients were treated with SDD. Most cultures were taken from the digestive tract (41.9%) and sputum (21.1%). A total of 20,593 isolates of AGNB were identified. The two most often found bacteria were Escherichia coli (N = 6409) and Pseudomonas (N = 5269). The incidence rate per 1000 patient-day for ICU-acquired resistance to cephalosporins was 2.03, for polymyxin B/colistin 0.51, for tobramycin 2.59 and for ciprofloxacin 2.2. The incidence rates for ICU-acquired resistant microbes per year ranged from 0 to 4.94 per 1000 patient-days, and no significant time-trend in incidence rates were found for any of the antimicrobials. The background prevalence rates of resistant strains measured on admission for cephalosporins, polymyxin B/colistin and ciprofloxacin rose over time with 7.9%, 3.5% and 8.0% respectively.
Conclusions
During more than 21-year SDD, the incidence rates of resistant microbes at the ICU level did not significantly increase over time but the background resistance rates increased. An overall ecological effect of prolonged application of SDD by counting resistant microorganisms in the ICU was not shown in a country with relatively low rates of resistant microorganisms.
Surmortalité >10% en cas de mauvais diagnostic de la porte d’entrée infectieuse
Abe et al. Critical Care 2019;23:202
Background
Rapid detection, early resuscitation, and appropriate antibiotic use are crucial for sepsis care. Accurate identification of the site of infection may facilitate a timely provision of appropriate care. We aimed to investigate the relationship between misdiagnosis of the site of infection at initial examination and in-hospital mortality.
Methods
This was a secondary-multicenter prospective cohort study involving 37 emergency departments. Consecutive adult patients with infection from December 2017 to February 2018 were included. Misdiagnosis of the site of infection was defined as a discrepancy between the suspected site of infection at initial examination and that at final diagnosis, including those infections remaining unidentified during hospital admission, whereas correct diagnosis was defined as site concordance. In-hospital mortality was compared between those misdiagnosed and those correctly diagnosed.
Results
Of 974 patients included in the analysis, 11.6% were misdiagnosed. Patients diagnosed with lung, intra-abdominal, urinary, soft tissue, and CNS infection at the initial examination, 4.2%, 3.8%, 13.6%, 10.9%, and 58.3% respectively, turned out to have an infection at a different site. In-hospital mortality occurred in 15%. In both generalized estimating equation (GEE) and propensity score-matched models, misdiagnosed patients exhibited higher mortality despite adjustment for patient background, site infection, and severity. The adjusted odds ratios (misdiagnosis vs. correct diagnosis) for in-hospital mortality were 2.66 (95% CI, 1.45–4.89) in the GEE model and 3.03 (95% CI, 1.24–7.38) in the propensity score-matched model. The difference in the absolute risk in the GEE model was 0.11 (0.04–0.18).
Conclusions
Among patients with infection, misdiagnosed site of infection is associated with a > 10% increase in in-hospital mortality.
Remplissage en débit libre versus débit lent : pas plus de fuite capillaire ?
Statkevicius et al. Critical Care 2019;23:191
Background
Optimal infusion rate of colloids in patients with suspected hypovolemia is unknown, and the primary objective of the present study was to test if plasma volume expansion by 5% albumin is greater if fluid is administered slowly rather than rapidly.
Methods
Patients with signs of hypoperfusion after major abdominal surgery were randomized to intravenous infusion of 5% albumin at a dose of 10 ml/kg (ideal body weight) either rapidly (30 min) or slowly (180 min). Plasma volume was measured using radiolabeled albumin at baseline, at 30 min, and at 180 min after the start of infusion. Primary outcome was change in plasma volume from the start of infusion to 180 min after the start of infusion. Secondary outcomes included the change in the area under the plasma volume curve and transcapillary escape rate (TER) for albumin from 180 to 240 min after the start of albumin infusion.
Results
A total of 33 and 31 patients were included in the analysis in the slow and rapid groups, respectively. The change in plasma volume from the start of infusion to 180 min did not differ between the slow and rapid infusion groups (7.4 ± 2.6 vs. 6.5 ± 4.1 ml/kg; absolute difference, 0.9 ml/kg [95%CI, − 0.8 to 2.6], P = 0.301). Change in the area under the plasma volume curve was smaller in the slow than in the rapid infusion group and was 866 ± 341 and 1226 ± 419 min ml/kg, respectively, P < 0.001. TER for albumin did not differ and was 5.3 ± 3.1%/h and 5.4 ± 3%/h in the slow and in the rapid infusion groups, respectively, P = 0.931.
Conclusions
This study does not support our hypothesis that a slow infusion of colloid results in a greater plasma volume expansion than a rapid infusion. Instead, our result of a smaller change in the area under the plasma volume curve indicates that a slow infusion results in a less efficient plasma volume expansion, but further studies are required to confirm this finding. A rapid infusion has no effect on vascular leak as measured after completion of the infusion.
Le Mottling score (score de marbrures) : bonnes capacités prédictives
Dumas et al. Critical Care 2019;23:211
Background
Mottling score, a tissue perfusion parameter, is correlated with outcome in septic shock patients. However, its predictive value on mortality according to prognostic covariates such as vasopressor dose and other tissue perfusion parameters remains unknown.
Methods
Mottling score and tissue perfusion parameters were recorded at ICU admission (H0), H-6, H 12, and H-24 and used to assess the predictive value of mottling score on 14-day mortality in a development cohort. Results were then validated in an independent cohort of septic shock patients in Brazil.
Results
Overall, 259 patients with sepsis or septic shock were included, 14-day mortality was 37%. Factors associated with death were mottling score (OR 2.26 [95% CI, 1.72–2.97]), arterial lactate level (OR 1.29 [1.11–1.5]), and urine output < 0.5 ml/Kg/h (OR 3.03 [1.37–6.69]). The C statistic for the model was 0.90 in the development cohort and 0.76 in the validation cohort. The predictive value of mottling score was not affected by vasopressor doses (p for interaction = 0.33): OR for mottling score ranged from 2.34 [1.10–3.15] in patients without vasopressor to 3.84 [1.98–7.43] in patients infused with high doses of vasopressor (> 0.8 μg/kg/min). There was no difference in the effect of mottling score on mortality according to mean arterial pressure, heart rate, cardiac index, and urine output, but we found a significant interaction between arterial lactate level and mottling score (p = 0.04). The predictive value of the mottling score remains significant when using the recent SEPSIS-3 definition of septic shock. Finally, a decrease of mottling score during resuscitation was significantly associated with better outcome after adjustment on SOFA score (p = 0.001).
Conclusions
Our results support the high prognostic value of mottling score for 14-day mortality in septic patients, whatever vasopressor dosage and other perfusion parameters. Mottling score variations during resuscitation are also predictive of mortality.
PCT : pas d’intérêt pour différencier les bactériémies des candidémies
Procalcitonin levels in candidemia versus bacteremia: a systematic review.
Cortegiani et al. Critical Care 2019;23:190
Revue et méta-analyse du choc septique dans les pays occidentaux
Vincent et al. Critical Care 2019;23:196
https://ccforum.biomedcentral.com/articles/10.1186/s13054-019-2478-6
Echec de l’écho diaphragmatique pour prédire l’echec d’extubation
Inability of Diaphragm Ultrasound to Predict Extubation Failure. A Multicenter Study.
https://journal.chestnet.org/article/S0012-3692(19)30694-4/pdf
DOI: https://doi.org/10.1016/j.chest.2019.03.004
Background
Diaphragmatic dysfunction may promote weaning difficulties in patients who are mechanically ventilated.
Objective
The goal of this study was to assess whether diaphragm dysfunction detected by ultrasound prior to extubation could predict extubation failure in the ICU.
Methods
This multicenter prospective study included patients at high risk of reintubation: those aged > 65 years, with underlying cardiac or respiratory disease, or intubated > 7 days. All patients had successfully undergone a spontaneous breathing trial. Diaphragmatic function was assessed by ultrasound prior to extubation while breathing spontaneously on a T-piece. Bilateral diaphragmatic excursion and apposition thickening fraction were measured, and diaphragmatic dysfunction was defined as excursion < 10 mm or thickening < 30%. Cough strength was clinically assessed by physiotherapists. Extubation failure was defined as reintubation or death within the 7 days following extubation.
Results
Over a 20-month period, 191 at-risk patients were studied. Among them, 33 (17%) were considered extubation failures. The proportion of patients with diaphragmatic dysfunction was similar between those whose extubation succeeded and those whose extubation failed: 46% vs 51% using excursion (P = .55), and 71% vs 68% using thickening (P = .73), respectively. Values of excursion and thickening did not differ between the success and the failure groups: at right, excursion was 14 ± 7 mm vs 11 ± 8 (P = .13), and thickening was 29 ± 29% vs 38 ± 48% (P = .83), respectively. Extubation failure rates were 7%, 22%, and 46% in patients with effective, moderate, and ineffective cough (P < .01). Ineffective cough was the only variable independently associated with extubation failure.
Conclusions
Diaphragmatic dysfunction assessed by ultrasound was not associated with an increased risk of extubation failure.
Quand le patient n’est pas d’accord sur son traitement en réa…
Antibiothérapie guidée par la PCT : vers la fin du débat ?
Levosimendan vs Milrinone en post-op de chirurgie cardiaque pédiatrique ?
et al., Ped CCM, 2019
https://insights.ovid.com/crossref?an=00130478-900000000-98211
DOI: 10.1097/PCC.0000000000002017
Objectives:It has been shown that, in contrast to other inotropic agents, levosimendan improves glomerular filtration rate after adult cardiac surgery. The aim of this study was to investigate the efficacy of levosimendan, compared with milrinone, in preventing acute kidney dysfunction in infants after open-heart surgery with cardiopulmonary bypass.
Design:Two-center, double-blinded, prospective, randomized clinical trial.
Setting:The study was performed in two tertiary pediatric centers, one in Sweden (Gothenburg) and one in Finland (Helsinki).
Patients:Infants between 1 and 12 months old, diagnosed with Tetralogy of Fallot, complete atrioventricular septal defect or nonrestrictive ventricular septal defect, undergoing total corrective cardiac surgery with cardiopulmonary bypass.
Interventions:Seventy-two infants were randomized to receive a perioperative infusion of levosimendan (0.1 µg/kg/min) or milrinone (0.4 µg/kg/min). The infusion was initiated at the start of cardiopulmonary bypass and continued for 26 hours.
Measurements and Main Results:The primary outcome variable was the absolute value of serum creatinine data on postoperative day 1. Secondary outcomes included the following: 1) acute kidney injury according to the serum creatinine criteria of the Kidney Diseases: Improving Global Outcomes; 2) acute kidney injury with serum creatinine corrected for fluid balance; 3) plasma neutrophil gelatinase-associated lipocalin; 4) cystatin C; 5) urea; 6) lactate; 7) hemodynamic variables; 8) use of diuretics in the PICU; 9) need of dialysis; 10) length of ventilator therapy; and 11) length of PICU stays. There was no significant difference in postoperative serum creatinine between the treatment groups over time (p = 0.65). The occurrence rate of acute kidney injury within 48 hours was 46.9% in the levosimendan group and 39.5% in the milrinone group (p = 0.70). There were no significant differences in other secondary outcome variables between the groups.
Conclusions:Levosimendan compared with milrinone did not reduce the occurrence rate of acute kidney injury in infants after total corrective heart surgery for atrioventricular septal defect, ventricular septal defect, or Tetralogy of Fallot.
Triage des patients pour la réa :
– Impact du délai du tri
Stohl et al. J Crit Care 2019;53:11-17
https://doi.org/10.1016/j.jcrc.2019.05.013
– Chez les patients d’onco-réa
Variability in triage practices for critically ill cancer patients: A randomized controlled trial.
https://doi.org/10.1016/j.jcrc.2019.05.012
Recommendations USA pour l’EP
Rivera-Lebron et al. Clinical and Applied Thrombosis/Hemostasis 2019;25:1-16
Kétamine comme anti-dépressif
Objective:
Subanesthetic ketamine doses have been shown to have rapid yet transient antidepressant effects in patients with treatment-resistant depression, which may be prolonged by repeated administration. The purpose of this study was to evaluate the antidepressant effects of a single ketamine infusion, a series of repeated ketamine infusions, and prolongation of response with maintenance infusions.
Methods:
Forty-one participants with treatment-resistant depression completed a single-site randomized double-blind crossover comparison of single infusions of ketamine and midazolam (an active placebo control). After relapse of depressive symptoms, participants received a course of six open-label ketamine infusions administered thrice weekly over 2 weeks. Responders, classified as those participants who had a ≥50% decrease in their scores on the Montgomery-Åsberg Depression Rating Scale (MADRS), received four additional infusions administered once weekly (maintenance phase).
Results:
Compared with midazolam, a single ketamine infusion elicited a significantly greater reduction in depressive symptoms at the primary efficacy endpoint (24 hours postinfusion). Linear mixed models revealed cumulative antidepressant effects with repeated infusions and doubling of the antidepressant response rate. Fifty-nine percent of participants met response criteria after repeated infusions, with a median of three infusions required before achieving response. Participants had no further change in MADRS scores during weekly maintenance infusions.
Conclusions:
Repeated ketamine infusions have cumulative and sustained antidepressant effects. Reductions in depressive symptoms were maintained among responders through once-weekly infusions. These findings provide novel data on efficacious administration strategies for ketamine in patients with treatment-resistant depression. Future studies should further expand on optimizing administration to better translate the use of ketamine into clinical settings.





 22 juillet 2019
22 juillet 2019















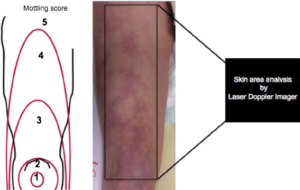


 Étiquettes :
Étiquettes :