Biblio du mois : Mai 2018
Here comes the new biblio du mois de l’AJAR ! Pour les plus réfractaires à l’anglais et pour vous tenir au courant, quelques petites astuces : ici
Au programme de ce mois-ci, de nombreuses études sur l’une de vos suppléances préférées : l’étude de l’ECMO précoce vs traitement conventionnel, l’étude RESTORE, des études sur les impacts de l’ECMO et de la prédiction de mortalité. On parlera également physio, de catécholamines avec une nouvelle étude qui remet l’accent sur l’intérêt de la Vasopressine dans le choc septique et des revues sur l’ACR, des recommandations de l’ACC sur la prise en charge des hémorragies sous anticoagulants oraux et bien d’autres !
Nous avons décidé de vous dédier une bonne partie à la prise en charge péri-opératoire et des articles/belles revues sur la méthodologie des essais cliniques en Anesthésie !
Vive l’Anesthésie-Réanimation !
ECMO précoce versus traitement conventionnel bien conduit dans le SDRA (très) sévère
Alain Combes, et al., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMoa1800385
DOI: 10.1056/NEJMoa1800385
Background
The efficacy of venovenous extracorporeal membrane oxygenation (ECMO) in patients with severe acute respiratory distress syndrome (ARDS) remains controversial.
Methods
In an international clinical trial, we randomly assigned patients with very severe ARDS, as indicated by one of three criteria — a ratio of partial pressure of arterial oxygen (Pao2) to the fraction of inspired oxygen (Fio2) of less than 50 mm Hg for more than 3 hours; a Pao2:Fio2 of less than 80 mm Hg for more than 6 hours; or an arterial blood pH of less than 7.25 with a partial pressure of arterial carbon dioxide of at least 60 mm Hg for more than 6 hours — to receive immediate venovenous ECMO (ECMO group) or continued conventional treatment (control group). Crossover to ECMO was possible for patients in the control group who had refractory hypoxemia. The primary end point was mortality at 60 days.
Results
At 60 days, 44 of 124 patients (35%) in the ECMO group and 57 of 125 (46%) in the control group had died (relative risk, 0.76; 95% confidence interval [CI], 0.55 to 1.04; P=0.09). Crossover to ECMO occurred a mean (±SD) of 6.5±9.7 days after randomization in 35 patients (28%) in the control group, with 20 of these patients (57%) dying. The frequency of complications did not differ significantly between groups, except that there were more bleeding events leading to transfusion in the ECMO group than in the control group (in 46% vs. 28% of patients; absolute risk difference, 18 percentage points; 95% CI, 6 to 30) as well as more cases of severe thrombocytopenia (in 27% vs. 16%; absolute risk difference, 11 percentage points; 95% CI, 0 to 21) and fewer cases of ischemic stroke (in no patients vs. 5%; absolute risk difference, −5 percentage points; 95% CI, −10 to −2).
Conclusions
Among patients with very severe ARDS, 60-day mortality was not significantly lower with ECMO than with a strategy of conventional mechanical ventilation that included ECMO as rescue therapy.
Attention à la stratégie de remplissage restrictive en chirurgie abdominale ?
Myles et al., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMoa1801601?query=nephrology
DOI: 10.1056/NEJMoa1801601
BACKGROUND
Guidelines to promote the early recovery of patients undergoing major surgery recommend a restrictive intravenous-fluid strategy for abdominal surgery. However, the supporting evidence is limited, and there is concern about impaired organ perfusion.
METHODS
In a pragmatic, international trial, we randomly assigned 3000 patients who had an increased risk of complications while undergoing major abdominal surgery to receive a restrictive or liberal intravenous-fluid regimen during and up to 24 hours after surgery. The primary outcome was disability-free survival at 1 year. Key secondary outcomes were acute kidney injury at 30 days, renal-replacement therapy at 90 days, and a composite of septic complications, surgical-site infection, or death.
RESULTS
During and up to 24 hours after surgery, 1490 patients in the restrictive fluid group had a median intravenous-fluid intake of 3.7 liters (interquartile range, 2.9 to 4.9), as compared with 6.1 liters (interquartile range, 5.0 to 7.4) in 1493 patients in the liberal fluid group (P<0.001). The rate of disability-free survival at 1 year was 81.9% in the restrictive fluid group and 82.3% in the liberal fluid group (hazard ratio for death or disability, 1.05; 95% confidence interval, 0.88 to 1.24; P=0.61). The rate of acute kidney injury was 8.6% in the restrictive fluid group and 5.0% in the liberal fluid group (P<0.001). The rate of septic complications or death was 21.8% in the restrictive fluid group and 19.8% in the liberal fluid group (P=0.19); rates of surgical-site infection (16.5% vs. 13.6%, P=0.02) and renal-replacement therapy (0.9% vs. 0.3%, P=0.048) were higher in the restrictive fluid group, but the between-group difference was not significant after adjustment for multiple testing.
CONCLUSIONS
Among patients at increased risk for complications during major abdominal surgery, a restrictive fluid regimen was not associated with a higher rate of disability-free survival than a liberal fluid regimen and was associated with a higher rate of acute kidney injury.
Echec de la PCT pour guider les infections pulmonaires ?
Huang et al., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMoa1802670?query=emergency-medicine
BACKGROUND
The effect of procalcitonin-guided use of antibiotics on treatment for suspected lower respiratory tract infection is unclear.
METHODS
In 14 U.S. hospitals with high adherence to quality measures for the treatment of pneumonia, we provided guidance for clinicians about national clinical practice recommendations for the treatment of lower respiratory tract infections and the interpretation of procalcitonin assays. We then randomly assigned patients who presented to the emergency department with a suspected lower respiratory tract infection and for whom the treating physician was uncertain whether antibiotic therapy was indicated to one of two groups: the procalcitonin group, in which the treating clinicians were provided with real-time initial (and serial, if the patient was hospitalized) procalcitonin assay results and an antibiotic use guideline with graded recommendations based on four tiers of procalcitonin levels, or the usual-care group. We hypothesized that within 30 days after enrollment the total antibiotic-days would be lower — and the percentage of patients with adverse outcomes would not be more than 4.5 percentage points higher — in the procalcitonin group than in the usual-care group.
RESULTS
A total of 1656 patients were included in the final analysis cohort (826 randomly assigned to the procalcitonin group and 830 to the usual-care group), of whom 782 (47.2%) were hospitalized and 984 (59.4%) received antibiotics within 30 days. The treating clinician received procalcitonin assay results for 792 of 826 patients (95.9%) in the procalcitonin group (median time from sample collection to assay result, 77 minutes) and for 18 of 830 patients (2.2%) in the usual-care group. In both groups, the procalcitonin-level tier was associated with the decision to prescribe antibiotics in the emergency department. There was no significant difference between the procalcitonin group and the usual-care group in antibiotic-days (mean, 4.2 and 4.3 days, respectively; difference, −0.05 day; 95% confidence interval [CI], −0.6 to 0.5; P=0.87) or the proportion of patients with adverse outcomes (11.7% [96 patients] and 13.1% [109 patients]; difference, −1.5 percentage points; 95% CI, −4.6 to 1.7; P<0.001 for noninferiority) within 30 days.
CONCLUSIONS
The provision of procalcitonin assay results, along with instructions on their interpretation, to emergency department and hospital-based clinicians did not result in less use of antibiotics than did usual care among patients with suspected lower respiratory tract infection.
Vers une thrombolyse guidée par l’IRM dans les AVC ischémiques non datés ?
Thomalla et al., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMoa1804355?query=emergency-medicine
DOI: 10.1056/NEJMoa1804355
BACKGROUND
Under current guidelines, intravenous thrombolysis is used to treat acute stroke only if it can be ascertained that the time since the onset of symptoms was less than 4.5 hours. We sought to determine whether patients with stroke with an unknown time of onset and features suggesting recent cerebral infarction on magnetic resonance imaging (MRI) would benefit from thrombolysis with the use of intravenous alteplase.
METHODS
In a multicenter trial, we randomly assigned patients who had an unknown time of onset of stroke to receive either intravenous alteplase or placebo. All the patients had an ischemic lesion that was visible on MRI diffusion-weighted imaging but no parenchymal hyperintensity on fluid-attenuated inversion recovery (FLAIR), which indicated that the stroke had occurred approximately within the previous 4.5 hours. We excluded patients for whom thrombectomy was planned. The primary end point was favorable outcome, as defined by a score of 0 or 1 on the modified Rankin scale of neurologic disability (which ranges from 0 [no symptoms] to 6 [death]) at 90 days. A secondary outcome was the likelihood that alteplase would lead to lower ordinal scores on the modified Rankin scale than would placebo (shift analysis).
RESULTS
The trial was stopped early owing to cessation of funding after the enrollment of 503 of an anticipated 800 patients. Of these patients, 254 were randomly assigned to receive alteplase and 249 to receive placebo. A favorable outcome at 90 days was reported in 131 of 246 patients (53.3%) in the alteplase group and in 102 of 244 patients (41.8%) in the placebo group (adjusted odds ratio, 1.61; 95% confidence interval [CI], 1.09 to 2.36; P=0.02). The median score on the modified Rankin scale at 90 days was 1 in the alteplase group and 2 in the placebo group (adjusted common odds ratio, 1.62; 95% CI, 1.17 to 2.23; P=0.003). There were 10 deaths (4.1%) in the alteplase group and 3 (1.2%) in the placebo group (odds ratio, 3.38; 95% CI, 0.92 to 12.52; P=0.07). The rate of symptomatic intracranial hemorrhage was 2.0% in the alteplase group and 0.4% in the placebo group (odds ratio, 4.95; 95% CI, 0.57 to 42.87; P=0.15).
CONCLUSIONS
In patients with acute stroke with an unknown time of onset, intravenous alteplase guided by a mismatch between diffusion-weighted imaging and FLAIR in the region of ischemia resulted in a significantly better functional outcome and numerically more intracranial hemorrhages than placebo at 90 days.
Pontage coronarien avec des artères radiales ?
Gaudino et al., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMoa1716026?query=cardiology
DOI: 10.1056/NEJMoa1716026
BACKGROUND
The use of radial-artery grafts for coronary-artery bypass grafting (CABG) may result in better postoperative outcomes than the use of saphenous-vein grafts. However, randomized, controlled trials comparing radial-artery grafts and saphenous-vein grafts have been individually underpowered to detect differences in clinical outcomes. We performed a patient-level combined analysis of randomized, controlled trials to compare radial-artery grafts and saphenous-vein grafts for CABG.
METHODS
Six trials were identified. The primary outcome was a composite of death, myocardial infarction, or repeat revascularization. The secondary outcome was graft patency on follow-up angiography. Mixed-effects Cox regression models were used to estimate the treatment effect on the outcomes.
RESULTS
A total of 1036 patients were included in the analysis (534 patients with radial-artery grafts and 502 patients with saphenous-vein grafts). After a mean (±SD) follow-up time of 60±30 months, the incidence of adverse cardiac events was significantly lower in association with radial-artery grafts than with saphenous-vein grafts (hazard ratio, 0.67; 95% confidence interval [CI], 0.49 to 0.90; P=0.01). At follow-up angiography (mean follow-up, 50±30 months), the use of radial-artery grafts was also associated with a significantly lower risk of occlusion (hazard ratio, 0.44; 95% CI, 0.28 to 0.70; P<0.001). As compared with the use of saphenous-vein grafts, the use of radial-artery grafts was associated with a nominally lower incidence of myocardial infarction (hazard ratio, 0.72; 95% CI, 0.53 to 0.99; P=0.04) and a lower incidence of repeat revascularization (hazard ratio, 0.50; 95% CI, 0.40 to 0.63; P<0.001) but not a lower incidence of death from any cause (hazard ratio, 0.90; 95% CI, 0.59 to 1.41; P=0.68).
CONCLUSIONS
As compared with the use of saphenous-vein grafts, the use of radial-artery grafts for CABG resulted in a lower rate of adverse cardiac events and a higher rate of patency at 5 years of follow-up.
Revue sur le syndrome des anti-phospholipides
David Garcia, M.D., and Doruk Erkan, M.D., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMra1705454
DOI: 10.1056/NEJMra1705454
Comment améliorer la qualité des greffons ? Une revue sur les stratégies actuelles et à venir
Stefan G. Tullius, M.D., Ph.D., and Hamid Rabb, M.D., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMra1507080
DOI: 10.1056/NEJMra1507080
Revue sur la fibrose pulmonaire idiopathique
David J. Lederer, M.D., and Fernando J. Martinez, M.D., NEJM, 2018
https://www.nejm.org/doi/full/10.1056/NEJMra1705751
DOI: 10.1056/NEJMra1705751
Acide Tranexamique dans l’AVC hémorragique : Non significatif sur la récupération fonctionnelle à J90
Sprigg et al., Lancet, 2018
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31033-X/fulltext
DOI: https://doi.org/10.1016/S0140-6736(18)31033-X
Background
Tranexamic acid can prevent death due to bleeding after trauma and post-partum haemorrhage. We aimed to assess whether tranexamic acid reduces haematoma expansion and improves outcome in adults with stroke due to intracerebral haemorrhage.
Methods
We did an international, randomised placebo-controlled trial in adults with intracerebral haemorrhage from acute stroke units at 124 hospital sites in 12 countries. Participants were randomly assigned (1:1) to receive 1 g intravenous tranexamic acid bolus followed by an 8 h infusion of 1 g tranexamic acid or a matching placebo, within 8 h of symptom onset. Randomisation was done centrally in real time via a secure website, with stratification by country and minimisation on key prognostic factors. Treatment allocation was concealed from patients, outcome assessors, and all other health-care workers involved in the trial. The primary outcome was functional status at day 90, measured by shift in the modified Rankin Scale, using ordinal logistic regression with adjustment for stratification and minimisation criteria. All analyses were done on an intention-to-treat basis. This trial is registered with the ISRCTN registry, number ISRCTN93732214.
Findings
We recruited 2325 participants between March 1, 2013, and Sept 30, 2017. 1161 patients received tranexamic acid and 1164 received placebo; the treatment groups were well balanced at baseline. The primary outcome was assessed for 2307 (99%) participants. The primary outcome, functional status at day 90, did not differ significantly between the groups (adjusted odds ratio [aOR] 0·88, 95% CI 0·76–1·03, p=0·11). Although there were fewer deaths by day 7 in the tranexamic acid group (101 [9%] deaths in the tranexamic acid group vs 123 [11%] deaths in the placebo group; aOR 0·73, 0·53–0·99, p=0·0406), there was no difference in case fatality at 90 days (250 [22%] vs 249 [21%]; adjusted hazard ratio 0·92, 95% CI 0·77–1·10, p=0·37). Fewer patients had serious adverse events after tranexamic acid than after placebo by days 2 (379 [33%] patients vs 417 [36%] patients), 7 (456 [39%] vs 497 [43%]), and 90 (521 [45%] vs 556 [48%]).
Interpretation
Functional status 90 days after intracerebral haemorrhage did not differ significantly between patients who received tranexamic acid and those who received placebo, despite a reduction in early deaths and serious adverse events. Larger randomised trials are needed to confirm or refute a clinically significant treatment effect.
La dyspnée, un symptôme encore peu considéré : quelques mots d’un médecin malade
Carel et al., Lancet, 2018
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(18)30106-1/fulltext
https://doi.org/10.1016/S2213-2600(18)30106-1
Vasopressine + Noradrénaline > Noradrénaline seule dans les chocs distributifs avec AC/FA ?
Mc Intyre et al., JAMA, 2018
https://jamanetwork.com/journals/jama/article-abstract/2680546
Importance
Vasopressin is an alternative to catecholamine vasopressors for patients with distributive shock—a condition due to excessive vasodilation, most frequently from severe infection. Blood pressure support with a noncatecholamine vasopressor may reduce stimulation of adrenergic receptors and decrease myocardial oxygen demand. Atrial fibrillation is common with catecholamines and is associated with adverse events, including mortality and increased length of stay (LOS).
Objectives
To determine whether treatment with vasopressin + catecholamine vasopressors compared with catecholamine vasopressors alone was associated with reductions in the risk of adverse events.
Data Sources
MEDLINE, EMBASE, and CENTRAL were searched from inception to February 2018. Experts were asked and meta-registries searched to identify ongoing trials.
Study Selection
Pairs of reviewers identified randomized clinical trials comparing vasopressin in combination with catecholamine vasopressors to catecholamines alone for patients with distributive shock.
Data Extraction and Synthesis
Two reviewers abstracted data independently. A random-effects model was used to combine data.
Main Outcomes and Measures
The primary outcome was atrial fibrillation. Other outcomes included mortality, requirement for renal replacement therapy (RRT), myocardial injury, ventricular arrhythmia, stroke, and LOS in the intensive care unit and hospital. Measures of association are reported as risk ratios (RRs) for clinical outcomes and mean differences for LOS.
Results
Twenty-three randomized clinical trials were identified (3088 patients; mean age, 61.1 years [14.2]; women, 45.3%). High-quality evidence supported a lower risk of atrial fibrillation associated with vasopressin treatment (RR, 0.77 [95% CI, 0.67 to 0.88]; risk difference [RD], −0.06 [95% CI, −0.13 to 0.01]). For mortality, the overall RR estimate was 0.89 (95% CI, 0.82 to 0.97; RD, −0.04 [95% CI, −0.07 to 0.00]); however, when limited to trials at low risk of bias, the RR estimate was 0.96 (95% CI, 0.84 to 1.11). The overall RR estimate for RRT was 0.74 (95% CI, 0.51 to 1.08; RD, −0.07 [95% CI, −0.12 to −0.01]). However, in an analysis limited to trials at low risk of bias, RR was 0.70 (95% CI, 0.53 to 0.92, P for interaction = .77). There were no significant differences in the pooled risks for other outcomes.
Conclusions and Relevance
In this systematic review and meta-analysis, the addition of vasopressin to catecholamine vasopressors compared with catecholamines alone was associated with a lower risk of atrial fibrillation. Findings for secondary outcomes varied.
Pour la fermeture de l’auricule gauche en per-opératoire de chirurgie cardiaque ?
Yao et al., JAMA, 2018
https://jamanetwork.com/journals/jama/article-abstract/2681747
Importance
Surgical occlusion of the left atrial appendage (LAAO) may be performed during concurrent cardiac surgery. However, few data exist on the association of LAAO with long-term risk of stroke, and some evidence suggests that this procedure may be associated with subsequent development of atrial fibrillation (AF).
Objective
To evaluate the association of surgical LAAO performed during cardiac surgery with risk of stroke, mortality, and development of subsequent AF.
Design, Setting, and Participants
Retrospective cohort study using a large US administrative database that contains data from adult patients (≥18 years) with private insurance or Medicare Advantage who underwent coronary artery bypass graft (CABG) or valve surgery between January 1, 2009, and March 30, 2017, with final follow-up on March 31, 2017. One-to-one propensity score matching was used to balance patients on 76 dimensions to compare those with vs without LAAO, stratified by history of prior AF at the time of surgery.
Exposures
Surgical LAAO vs no surgical LAAO during cardiac surgery.
Main Outcomes and Measures
The primary outcomes were stroke (ie, ischemic stroke or systemic embolism) and all-cause mortality. The secondary outcomes were postoperative AF (AF within 30 days after surgery among patients without prior AF) and long-term AF-related health utilization (event rates of outpatient visits and hospitalizations).
Results
Among 75 782 patients who underwent cardiac surgery (mean age, 66.0 [SD, 11.2] years; 2 2091 [29.2%] women, 25 721 [33.9%] with preexisting AF), 4374 (5.8%) underwent concurrent LAAO, and mean follow-up was 2.1 (SD, 1.9) years. In the 8590 propensity score–matched patients, LAAO was associated with a reduced risk of stroke (1.14 vs 1.59 events per 100 person-years; hazard ratio [HR], 0.73 [95% CI, 0.56-0.96]; P = .03) and mortality (3.01 vs 4.30 events per 100 person-years; HR, 0.71 [95% CI, 0.60-0.84]; P < .001). LAAO was associated with higher rates of AF-related outpatient visits (11.96 vs 10.26 events per person-year; absolute difference, 1.70 [95% CI, 1.60-1.80] events per person-year; rate ratio, 1.17 [95% CI, 1.10-1.24]; P < .001) and hospitalizations (0.36 vs 0.32 event per person-year; absolute difference, 0.04 [95% CI, 0.02-0.06] event per person-year; rate ratio, 1.13 [95% CI, 1.05-1.21]; P = .002). In patients with prior AF (6438/8590 [74.9%]) with vs without LAAO, risk of stroke was 1.11 vs 1.71 events per 100 person-years (HR, 0.68 [95% CI, 0.50-0.92]; P = .01) and risk of mortality was 3.22 vs 4.93 events per 100 person-years (HR, 0.67 [95% CI, 0.56-0.80]; P < .001), respectively. In patients without prior AF (2152/8590 [25.1%]) with vs without LAAO, risk of stroke was 1.23 vs 1.26 events per 100 person-years (HR, 0.95 [95% CI, 0.54-1.68]), risk of mortality was 2.30 vs 2.49 events per 100 person-years (HR, 0.92 [95% CI, 0.61-1.37]), and risk of postoperative AF was 27.7% vs 20.2% events per 100 person-years (HR, 1.46 [95% CI, 1.22-1.73]; P < .001). The interaction term between prior AF and LAAO was not significant (P = .29 for stroke and P = .16 for mortality).
Conclusions and Relevance
Among patients undergoing cardiac surgery, concurrent surgical LAAO, compared with no surgical LAAO, was associated with reduced risk of subsequent stroke and all-cause mortality. Further research, including from randomized clinical trials, is needed to more definitively determine the role of surgical LAAO.
Recommandations sur la prise en charge de syndrome hémorragique sous anticoagulants
https://jamanetwork.com/journals/jama/article-abstract/2681178
Les « drapeaux rouges » de l’hémorragie d’origine traumatique :
– PAM<70mmHg,
– Hb<13g/dL,
– pelvis instable,
– intubation pré-hospitalière,
– shock index (FC/PAS) > 1
Sophie Rym Hamada, et al., Critical Care 2018
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2026-9
https://doi.org/10.1186/
Background
Haemorrhagic shock is the leading cause of early preventable death in severe trauma. Delayed treatment is a recognized prognostic factor that can be prevented by efficient organization of care. This study aimed to develop and validate Red Flag, a binary alert identifying blunt trauma patients with high risk of severe haemorrhage (SH), to be used by the pre-hospital trauma team in order to trigger an adequate intra-hospital standardized haemorrhage control response: massive transfusion protocol and/or immediate haemostatic procedures.
Methods
A multicentre retrospective study of prospectively collected data from a trauma registry (Traumabase®) was performed. SH was defined as: packed red blood cell (RBC) transfusion in the trauma room, or transfusion ≥ 4 RBC in the first 6 h, or lactate ≥ 5 mmol/L, or immediate haemostatic surgery, or interventional radiology and/or death of haemorrhagic shock. Pre-hospital characteristics were selected using a multiple logistic regression model in a derivation cohort to develop a Red Flag binary alert whose performances were confirmed in a validation cohort.
Results
Among the 3675 patients of the derivation cohort, 672 (18%) had SH. The final prediction model included five pre-hospital variables: Shock Index ≥ 1, mean arterial blood pressure ≤ 70 mmHg, point of care haemoglobin ≤ 13 g/dl, unstable pelvis and pre-hospital intubation. The Red Flag alert was triggered by the presence of any combination of at least two criteria. Its predictive performances were sensitivity 75% (72–79%), specificity 79% (77–80%) and area under the receiver operating characteristic curve 0.83 (0.81–0.84) in the derivation cohort, and were not significantly different in the independent validation cohort of 2999 patients.
Conclusion
The Red Flag alert developed and validated in this study has high performance to accurately predict or exclude SH.
Revues sur l’Arrêt cardio-respiratoire :
– sur les dispositifs de compression mécanique
Mechanical CPR: Who? When? How?
Kurtis Poole, et al., Critical Care 2018 22:140
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2059-0
https://doi.org/10.1186/
In cardiac arrest, high quality cardiopulmonary resuscitation (CPR) is a key determinant of patient survival. However, delivery of effective chest compressions is often inconsistent, subject to fatigue and practically challenging.
Mechanical CPR devices provide an automated way to deliver high-quality CPR. However, large randomised controlled trials of the routine use of mechanical devices in the out-of-hospital setting have found no evidence of improved patient outcome in patients treated with mechanical CPR, compared with manual CPR. The limited data on use during in-hospital cardiac arrest provides preliminary data supporting use of mechanical devices, but this needs to be robustly tested in randomised controlled trials.
In situations where high-quality manual chest compressions cannot be safely delivered, the use of a mechanical device may be a reasonable clinical approach. Examples of such situations include ambulance transportation, primary percutaneous coronary intervention, as a bridge to extracorporeal CPR and to facilitate uncontrolled organ donation after circulatory death.
The precise time point during a cardiac arrest at which to deploy a mechanical device is uncertain, particularly in patients presenting in a shockable rhythm. The deployment process requires interruptions in chest compression, which may be harmful if the pause is prolonged. It is recommended that use of mechanical devices should occur only in systems where quality assurance mechanisms are in place to monitor and manage pauses associated with deployment.
In summary, mechanical CPR devices may provide a useful adjunct to standard treatment in specific situations, but current evidence does not support their routine use.
– sur l’adrénaline
The role of adrenaline in cardiopulmonary resuscitation
Christopher J. R. Gough and Jerry P. Nolan, Critical Care 2018 22:139
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2058-1
https://doi.org/10.1186/
Adrenaline has been used in the treatment of cardiac arrest for many years. It increases the likelihood of return of spontaneous circulation (ROSC), but some studies have shown that it impairs cerebral microcirculatory flow. It is possible that better short-term survival comes at the cost of worse long-term outcomes. This narrative review summarises the rationale for using adrenaline, significant studies to date, and ongoing research.
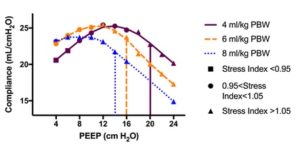
La meilleure PEEP dépend du volume courant !
Best PEEP trials are dependent on tidal volume
Determining the optimal positive end-expiratory pressure (PEEP) in patients with acute respiratory distress syndrome remains an area of active investigation. Most trials individualizing PEEP optimize one physiologic parameter (e.g., driving pressure) by titrating PEEP while holding other ventilator settings constant. Optimal PEEP, however, may depend on the tidal volume, and changing the tidal volume with which a best PEEP trial is performed may lead to different best PEEP settings in the same patient.
Réduction du délirium de réanimation par l’administration nocturne de Dexmedetomidine (étude SKY-DEX)
Rationale: Dexmedetomidine is associated with less delirium than benzodiazepines and better sleep architecture than either benzodiazepines or propofol; its effect on delirium and sleep when administered at night to patients requiring sedation remains unclear.
Objectives: To determine if nocturnal dexmedetomidine prevents delirium and improves sleep in critically ill adults.
Methods: This two-center, double-blind, placebo-controlled trial randomized 100 delirium-free critically ill adults receiving sedatives to receive nocturnal (9:30 p.m. to 6:15 a.m.) intravenous dexmedetomidine (0.2 μg/kg/h, titrated by 0.1 μg /kg/h every 15 min until a goal Richmond Agitation and Sedation Scale score of −1 or maximum rate of 0.7 μg/kg/h was reached) or placebo until ICU discharge. During study infusions, all sedatives were halved; opioids were unchanged. Delirium was assessed using the Intensive Care Delirium Screening Checklist every 12 hours throughout the ICU admission. Sleep was evaluated each morning by the Leeds Sleep Evaluation Questionnaire.
Measurements and Main Results: Nocturnal dexmedetomidine (vs. placebo) was associated with a greater proportion of patients who remained delirium-free during the ICU stay (dexmedetomidine [40 (80%) of 50 patients] vs. placebo [27 (54%) of 50 patients]; relative risk, 0.44; 95% confidence interval, 0.23–0.82; P = 0.006). The average Leeds Sleep Evaluation Questionnaire score was similar (mean difference, 0.02; 95% confidence interval, 0.42–1.92) between the 34 dexmedetomidine (average seven assessments per patient) and 30 placebo (six per patient) group patients able to provide one or more assessments. Incidence of hypotension, bradycardia, or both did not differ significantly between groups.
Conclusions: Nocturnal administration of low-dose dexmedetomidine in critically ill adults reduces the incidence of delirium during the ICU stay; patient-reported sleep quality appears unchanged.
Intérêt de l’ECMO dans le SDRA chez l’enfant ? (étude RESTORE)
Barbaro et al., AJRCCM, 2018
Rationale: Extracorporeal membrane oxygenation (ECMO) has supported gas exchange in children with severe respiratory failure for more than 40 years, without ECMO efficacy studies.
Objectives: To compare the mortality and functional status of children with severe acute respiratory failure supported with and without ECMO.
Methods: This cohort study compared ECMO-supported children to pair-matched non–ECMO-supported control subjects with severe acute respiratory distress syndrome (ARDS). Both individual case matching and propensity score matching were used. The study sample was selected from children enrolled in the cluster-randomized RESTORE (Randomized Evaluation of Sedation Titration for Respiratory Failure) clinical trial. Detailed demographic and daily physiologic data were used to match patients. The primary endpoint was in-hospital mortality. Secondary outcomes included hospital-free days, ventilator-free days, and change in functional status at hospital discharge.
Measurements and Main Results: Of 2,449 children in the RESTORE trial, 879 (35.9%) non–ECMO-supported patients with severe ARDS were eligible to match to 61 (2.5%) ECMO-supported children. When individual case matching was used (60 matched pairs), the in-hospital mortality rate at 90 days was 25% (15 of 60) for both the ECMO-supported and non–ECMO-supported children (P > 0.99). With propensity score matching (61 matched pairs), the ECMO-supported in-hospital mortality rate was 15 of 61 (25%), and the non–ECMO-supported hospital mortality rate was 18 of 61 (30%) (P = 0.70). There was no difference between ECMO-supported and non–ECMO-supported patients in any secondary outcomes.
Conclusions: In children with severe ARDS, our results do not demonstrate that ECMO-supported children have superior outcomes compared with non–ECMO-supported children. Definitive answers will require a rigorous multisite randomized controlled trial.
De fortes PEEP préviendraient les lésions pulmonaires induites en ventilation spontanée dans le SDRA ?
Morais et al., AJRCCM, 2018
Rationale: In acute respiratory distress syndrome (ARDS), atelectatic solid-like lung tissue impairs transmission of negative swings in pleural pressure (Ppl) that result from diaphragmatic contraction. The localization of more negative Ppl proportionally increases dependent lung stretch by drawing gas either from other lung regions (e.g., nondependent lung [pendelluft]) or from the ventilator. Lowering the level of spontaneous effort and/or converting solid-like to fluid-like lung might render spontaneous effort noninjurious.
Objectives: To determine whether spontaneous effort increases dependent lung injury, and whether such injury would be reduced by recruiting atelectatic solid-like lung with positive end-expiratory pressure (PEEP).
Methods: Established models of severe ARDS (rabbit, pig) were used. Regional histology (rabbit), inflammation (positron emission tomography; pig), regional inspiratory Ppl (intrabronchial balloon manometry), and stretch (electrical impedance tomography; pig) were measured. Respiratory drive was evaluated in 11 patients with ARDS.
Measurements and Main Results: Although injury during muscle paralysis was predominantly in nondependent and middle lung regions at low (vs. high) PEEP, strong inspiratory effort increased injury (indicated by positron emission tomography and histology) in dependent lung. Stronger effort (vs. muscle paralysis) caused local overstretch and greater tidal recruitment in dependent lung, where more negative Ppl was localized and greater stretch was generated. In contrast, high PEEP minimized lung injury by more uniformly distributing negative Ppl, and lowering the magnitude of spontaneous effort (i.e., deflection in esophageal pressure observed in rabbits, pigs, and patients).
Conclusions: Strong effort increased dependent lung injury, where higher local lung stress and stretch was generated; effort-dependent lung injury was minimized by high PEEP in severe ARDS, which may offset need for paralysis.
Facteurs de risque de syndrome confusionnel en post-opératoire de PTH/PTG : influence de l’anesthésie
Background
Postoperative delirium continues to pose major clinical difficulties. While unmodifiable factors (e.g. age and comorbidity burden) are commonly studied risk factors for delirium, the role of modifiable factors, such as anaesthesia type and commonly used perioperative medications, remains understudied. This study aims to evaluate the role of modifiable factors for delirium after hip and knee arthroplasties.
Methods
We performed a retrospective study of 41 766 patients who underwent hip or knee arthroplasties between 2005 and 2014 at a single institution. Data were collected as part of routine patient care. Multivariable logistic regression models assessed associations between anaesthesia type and commonly used perioperative medications (opioids, benzodiazepines, and ketamine) and postoperative delirium. Odds ratios (OR) and 95% confidence intervals (CI) are reported. Various sensitivity analyses are also considered, including multiple imputation methods to address missing data.
Results
Postoperative delirium occurred in 2.21% (n=922) of all patients. While patients who received neuraxial anaesthesia were at lower risk for postoperative delirium (compared with general anaesthesia; epidural OR 0.59 CI 0.38–0.93; spinal OR 0.55 CI 0.37–0.83; combined spinal/epidural OR 0.56 CI 0.40–0.80), those given intraoperative ketamine (OR 1.27 CI 1.01–1.59), opioids (OR 1.25 CI 1.09–1.44), postoperative benzodiazepines (OR 2.47 CI 2.04–2.97), and ketamine infusion (OR 10.59 CI 5.26–19.91) were at a higher risk.
Conclusions
In this cohort of hip and knee arthroplasty patients, anaesthesia type and perioperative medications were associated with increased odds for postoperative delirium. Our results support the notion that modifiable risk factors may exacerbate or attenuate risk for postoperative delirium.
Diminution des effets psychodysleptiques de la Kétamine par le NO ?
Background
Animal studies suggest that N-methyl-d-aspartate receptor (NMDAR) hypofunction and subsequent decline in intracellular nitric oxide (NO) are responsible for development of ketamine-induced psychedelic symptoms. To examine this mechanism in humans, we administered the NO donor sodium nitroprusside during infusion of racemic ketamine (RS-ketamine), containing equal amounts of S(+)- and R(–)-ketamine isomers, or esketamine, containing just the S(+)-isomer.
Methods
In this randomised, double blind, placebo-controlled crossover study, healthy volunteers were treated with sodium nitroprusside 0.5 μg kg−1 min−1 or placebo during administration of escalating doses of RS-ketamine (total dose 140 mg) or esketamine (70 mg). Drug high, internal and external perception, obtained using the Bowdle questionnaire, were scored over time on a visual analogue scale. The area-under-the-time-effect-curve (AUC) was calculated for each end-point.
Results
Sodium nitroprusside significantly reduced drug high AUC [mean (standard deviation); placebo 9070 (4630) vs sodium nitroprusside 7100 (3320), P=0.02], internal perception AUC [placebo 1310 (1250) vs nitroprusside 748 (786), P<0.01] and external perception AUC [placebo 4110 (2840) vs nitroprusside 2890 (2120), P=0.02] during RS-ketamine infusion, but was without effect on any of these measures during esketamine infusion.
Conclusions
These data suggest that NO depletion plays a role in RS-ketamine-induced psychedelic symptoms in humans. The sodium nitroprusside effect was observed for R(–)- but not S(+)-isomer-induced psychedelic symptoms. Further studies are needed to corroborate our findings and assess whether higher sodium nitroprusside doses will reduce esketamine-induced psychedelic symptoms.
Revue sur l’utilisation de la protamine en chirurgie cardiaque
Boer et al., BJA, 2018
Revue sur la gestion péri-opératoire de l’anémie en neurochirurgie
Kisilevsky et al., BJA, 2018
Revue et recommandations sur les définitions des complications respiratoire post-opératoires
Revue sur le manque de robustesse des essais cliniques en anesthésie
Mazzinari et al., BJA, 2018
Doit-on s’inquiéter des radiations en réanimation ?
Krishnan et al., Chest, 2018
DOI: https://doi.org/10.1016/j.chest.2018.01.019
Background
Patients admitted to the medical ICU (MICU) are often subjected to multiple radiologic studies. We hypothesized that some endure radiation dose exposure (cumulative effective dose [CED]) in excess of annual US federal occupational health standard limits (CED ≥ 50 mSv) and 5-year cumulative limit (CED ≥ 100 mSv). We also evaluated the correlation of CED with Acute Physiology and Chronic Health Evaluation (APACHE) III score and other clinical variables.
Methods
Retrospective observational study conducted in an academic medical center involving all adult admissions (N = 4,155) to the MICU between January 2013 and December 2013. Radiation doses from ionizing radiologic studies were calculated from reference values to determine the CED.
Results
Three percent of admissions (n = 131) accrued CED ≥ 50 mSv (1% [n = 47] accrued CED ≥ 100 mSv). The median CED was 0.72 mSv (interquartile range, 0.02-5.23 mSv), with a range of 0.00 to 323 mSv. Higher APACHE III scores (P = .003), longer length of MICU stay (P < .0001), sepsis (P = .03), and gastrointestinal disorders and bleeding (P < .0001) predicted higher CED in a multivariable linear regression model. Patients with gastrointestinal bleeding and disorders had an odds ratio of 21.05 (95% CI, 13.54-32.72; P < .0001) and 6.94 (95% CI, 3.88-12.38; P < .0001), respectively, of accruing CED ≥ 50 mSv in a multivariable logistic regression model. CT scan and interventional radiology accounted for 49% and 38% of the total CED, respectively.
Conclusions
Patients in the MICU are exposed to radiation doses that can be substantial, exceeding federal annual occupational limits, and in a select subset, are > 100 mSv. Efforts to justify, restrict, and optimize the use of radiologic resources when feasible are warranted.
Drainage d’un pneumothorax : queue de cochon ou drain de Joly ?
Chang et al., Chest, 2018
Background
The optimal initial treatment approach for pneumothorax remains controversial. This systemic review and meta-analysis investigated the effectiveness of small-bore pigtail catheter (PC) drainage compared with that of large-bore chest tube (LBCT) drainage as the initial treatment approach for all subtypes of pneumothorax.
Methods
PubMed and Embase were systematically searched for observational studies and randomized controlled trials published up to October 9, 2017, that compared PC and LBCT as the initial treatment for pneumothorax. The investigative outcomes included success rates, recurrence rates, complication rates, drainage duration, and hospital stay.
Results
Of the 11 included studies (875 patients), the success rate was similar in the PC (79.84%) and LBCT (82.87%) groups, with a risk ratio of 0.99 (95% CI, 0.93 to 1.05; I2 = 0%). Specifically, PC drainage was associated with a significantly lower complication rate following spontaneous pneumothorax than LBCT drainage (Peto odds ratio: 0.49 [95% CI, 0.28 to 0.85]; I2 = 29%). In the spontaneous subgroup, PC drainage was associated with a significantly shorter drainage duration (mean difference, −1.51 [95% CI, −2.93 to −0.09]) and hospital stay (mean difference: −2.54 [95% CI, −3.16 to −1.92]; P < .001) than the LBCT group.
Conclusions
Collectively, results of the meta-analysis suggest PC drainage may be considered as the initial treatment option for patients with primary or secondary spontaneous pneumothorax. Ideally, randomized controlled trials are needed to compare PC vs LBCT among different subgroups of patients with pneumothorax, which may ultimately improve clinical care and management for these patients.
Index Excursion diaphragmatique-temps inspiratoire : un nouveau paramètre d’échographie diaphragmatique pour prédire l’échec d’extubation ?
Palkar et al., Chest, 2018
Background
The diaphragmatic response to increased mechanical load following withdrawal of mechanical ventilation is critical in determining the outcome of extubation. Using ultrasonography, we aimed to evaluate the performance of the excursion-time (E-T) index—a product of diaphragm excursion and inspiratory time, to predict the outcome of extubation.
Methods
Right hemidiaphragm excursion, inspiratory time, and E-T index were measured by ultrasonography during mechanical ventilation: (1) on assist-control (A/C) mode during consistent patient-triggered ventilation, (2) following 30 min during a spontaneous breathing trial (SBT), and (3) between 4 and 24 h following extubation. These measurements were correlated with the outcome of extubation. Patients in the “failure” group required reintubation or noninvasive ventilation within 48 h of extubation.
Results
Of the 73 patients studied, 20 patients failed extubation. During SBT, diaphragm excursion was 1.65 ± 0.82 and 2.1 ± 0.9 cm (P = .06), inspiratory time was 0.89 ± 0.30 and 1.11 ± 0.39 s (P = .03), and the E-T index was 1.64 ± 1.19 and 2.42 ± 1.55 cm-s (P < .03) in the “failure” and “success” groups, respectively. The mean change in E-T index between A/C and SBT was –3.9 ± 57.8% in the failure group and 59.4 ± 74.6% in the success group (P < .01). A decrease in diaphragmatic E-T index less than 3.8% between A/C and SBT had a sensitivity of 79.2% and a specificity of 75%, to predict successful extubation.
Conclusions
Diaphragm E-T index measured during SBT may help predict the outcome of extubation. Maintenance or increase in diaphragm E-T index between A/C and SBT increases the likelihood of successful extubation.
Revue sur l’hémodynamique au cours de la tamponnade
Kearns et al., Chest, 2018
Nouveau score de gravité dans le sepsis : The New York Sepsis Severity Score
doi: 10.1097/CCM.0000000000002824
Objectives:
In accordance with Rory’s Regulations, hospitals across New York State developed andimplemented protocols for sepsis recognition and treatment to reduce variations in evidence informed care and preventable mortality. The New York Department of Health sought to develop a risk assessment model foraccurate and standardized hospital mortality comparisons of adult septic patients across institutions using case-mix adjustment.
Design:
Retrospective evaluation of prospectively collected data.
Patients:
Data from 43,204 severe sepsis and septic shock patients from 179 hospitals across New YorkState were evaluated.
Settings:
Prospective data were submitted to a database from January 1, 2015, to December 31, 2015.
Measurement and Main Results:
Maximum likelihood logistic regression was used to estimate modelcoefficients used in the New York State risk model. The mortality probability was estimated using a logisticregression model. Variables to be included in the model were determined as part of the model-building process. Interactions between variables were included if they made clinical sense and if their p values were less than 0.05. Model development used a random sample of 90% of available patients and was validated using the remaining10%. Hosmer-Lemeshow goodness of fit p values were considerably greater than 0.05, suggesting goodcalibration. Areas under the receiver operator curve in the developmental and validation subsets were 0.770 (95% CI, 0.765–0.775) and 0.773 (95% CI, 0.758–0.787), respectively, indicating good discrimination. Development andvalidation datasets had similar distributions of estimated mortality probabilities. Mortality increased with rising age, comorbidities, and lactate.
Conclusions:
The New York Sepsis Severity Score accurately estimated the probability of hospitalmortality in severe sepsis and septic shock patients. It performed well with respect to calibration anddiscrimination. This sepsis-specific model provides an accurate, comprehensive method for standardized mortalitycomparison of adult patients with severe sepsis and septic shock.
Augmentation de la morbi-mortalité avec la durée d’attente avant d’être admis en réanimation
Mathews et al., CCM, 2018
Objectives:
ICU admission delays can negatively affect patient outcomes, but emergency department volume and boarding times may also affect these decisions and associated patient outcomes. We sought to investigate the effect of emergency department and ICU capacity strain on ICU admission decisions and to examine the effect of emergency department boarding time of critically ill patients on in-hospital mortality.
Design:
A retrospective cohort study.
Setting:
Single academic tertiary care hospital.
Patients:
Adult critically ill emergency department patients for whom a consult for medical ICU admission was requested, over a 21-month period.
Interventions:
None.
Measurements and Main Results:
Patient data, including severity of illness (Mortality Probability Model III on Admission), outcomes of mortality and persistent organ dysfunction, and hourly census reports for the emergency department, for all ICUs and all adult wards were compiled. A total of 854 emergency department requests for ICU admission were logged, with 455 (53.3%) as “accept” and 399 (46.7%) as “deny” cases, with median emergency department boarding times 4.2 hours (interquartile range, 2.8–6.3 hr) and 11.7 hours (3.2–20.3 hr) and similar rates of persistent organ dysfunction and/or death 41.5% and 44.6%, respectively. Those accepted were younger (mean ± SD, 61 ± 17 vs 65 ± 18 yr) and more severely ill (median Mortality Probability Model III on Admission score, 15.3% [7.0–29.5%] vs 13.4% [6.3–25.2%]) than those denied admission. In the multivariable model, a full medical ICU was the only hospital-level factor significantly associated with a lower probability of ICU acceptance (odds ratio, 0.55 [95% CI, 0.37–0.81]). Using propensity score analysis to account for imbalances in baseline characteristics between those accepted or denied for ICU admission, longer emergency department boarding time after consult was associated with higher odds of mortality and persistent organ dysfunction (odds ratio, 1.77 [1.07–2.95]/log10 hour increase).
Conclusions:
ICU admission decisions for critically ill emergency department patients are affected by medical ICU bed availability, though higher emergency department volume and other ICU occupancy did not play a role. Prolonged emergency department boarding times were associated with worse patient outcomes, suggesting a need for improved throughput and targeted care for patients awaiting ICU admission.
Impact de la coagulopathie associé au sepsis sur la mortalité
Lyons et al., CCM, 2018
Objectives:
To assess whether sepsis-associated coagulopathy predicts hospital mortality.
Design:
Retrospective cohort study.
Setting:
One-thousand three-hundred beds urban academic medical center.
Patients:
Six-thousand one-hundred forty-eight consecutive patients hospitalized between January 1, 2010, and December 31, 2015.
Interventions:
Mild sepsis-associated coagulopathy was defined as an international normalized ratio greater than or equal to 1.2 and less than 1.4 plus platelet count less than or equal to 150,000/µL but greater than 100,000/µL; moderate sepsis-associated coagulopathy was defined with either an international normalized ratio greater than or equal to 1.4 but less than 1.6 or platelets less than or equal to 100,000/µL but greater than 80,000/µL; severe sepsis-associated coagulopathy was defined as an international normalized ratio greater than or equal to 1.6 and platelets less than or equal to 80,000/µL.
Measurements and Main Results:
Hospital mortality increased progressively from 25.4% in patients without sepsis-associated coagulopathy to 56.1% in patients with severe sepsis-associated coagulopathy. Similarly, duration of hospitalization and ICU care increased progressively as sepsis-associated coagulopathy severity increased. Multivariable analyses showed that the presence of sepsis-associated coagulopathy, as well as sepsis-associated coagulopathy severity, was independently associated with hospital mortality regardless of adjustments made for baseline patient characteristics, hospitalization variables, and the sepsis-associated coagulopathy-cancer interaction. Odds ratios ranged from 1.33 to 2.14 for the presence of sepsis-associated coagulopathy and from 1.18 to 1.51 for sepsis-associated coagulopathy severity for predicting hospital mortality (p < 0.001 for all comparisons).
Conclusions:
The presence of sepsis-associated coagulopathy identifies a group of patients with sepsis at higher risk for mortality. Furthermore, there is an incremental risk of mortality as the severity of sepsis-associated coagulopathy increases.
Autorégulation et ischémie cérébrale retardée dans l’hémorragie sous-arachnoïdienne
doi: 10.1097/CCM.0000000000003016
Objectives:
Pressure reactivity index and oxygen reactivity index are used to assess cerebral autoregulation after acute brain injury. The value of autoregulation indices in the prediction of delayed cerebral ischemia and outcome in patients with subarachnoid hemorrhage is still inconclusive. In this study, we aimed to focus on the predictive value of the first 72 hours commonly referred to as “early brain injury” in comparison to the overall monitoring period.
Design:
Retrospective observational cohort study.
Setting:
Neurocritical care unit at a tertiary academic medical center.
Patients:
Forty-three consecutive poor-grade patients with nontraumatic subarachnoid hemorrhage admitted between 2012 and 2016 undergoing continuous high-frequency monitoring.
Interventions:
High-frequency monitoring includes arterial blood pressure, intracranial pressure, and brain tissue oxygen tension. Pressure reactivity index and oxygen reactivity index were evaluated as moving correlation coefficient between mean arterial pressure/intracranial pressure and cerebral perfusion pressure/brain tissue oxygen tension, respectively.
Measurements and Main Results:
Median autoregulation monitoring time was 188 ± 91 hours per patient. Initial pressure reactivity index was 0.31 ± 0.02 and decreased significantly to 0.01 ± 0.01 (p < 0.001) 3 days after admission with a second peak 10 days after admission (0.18 ± 0.14; p = 0.001). Admission oxygen reactivity index was high, 0.25 ± 0.03, and decreased to a minimum of 0.11 ± 0.02 eight days after admission (p = 0.008). Patients with delayed cerebral ischemia had significantly higher overall mean pressure reactivity index values (p < 0.04), which were more pronounced during the first 72 hours, reflecting early brain injury (p < 0.02). High pressure reactivity index during the first 72 hours was associated with poor functional outcome (p < 0.001). No association between oxygen reactivity index and delayed cerebral ischemia or clinical outcome was observed (p = 0.8/0.78).
Conclusions:
High initial pressure reactivity index, presumably reflecting early brain injury, but not oxygen reactivity index, was associated with delayed cerebral ischemia and worse clinical outcome in poor-grade subarachnoid hemorrhage patients. Our data indicate that autoregulation indices should be interpreted cautiously when used in these patients and that timing is crucial when autoregulation indices are evaluated as predictor for delayed cerebral ischemia and outcome.
Séquelles cognitifs à long terme après ECMO
Objectives:
To investigate the presence of cognitive dysfunction and brain lesions in long-term survivors after treatment with extracorporeal membrane oxygenation for severe respiratory failure, and to see whether patients with prolonged hypoxemia were at increased risk.
Design:
A single-center retrospective cohort study.
Setting:
Tertiary referral center for extracorporeal membrane oxygenation in Sweden.
Patients:
Long-term survivors treated between 1995 and July 2009. Seven patients from a previously published study investigated with a similar protocol were included.
Interventions:
Brain imaging, neurocognitive testing, interview.
Measurements and Main Results:
Thirty-eight patients (i.e., n = 31 + 7) were enrolled and investigated in median 9.0 years after discharge. Only memory tests were performed in 10 patients, mainly due to a lack of formal education necessary for the test results to be reliable. Median full-scale intelligence quotient, memory index, and executive index were 97, 101, and 104, respectively (normal, 100 ± 15). Cognitive function was not reduced in the group with prolonged hypoxemia. Brain imaging showed cerebrovascular lesions in 14 of 38 patients (37%), most commonly in the group treated with venoarterial extracorporeal membrane oxygenation (7/11, 64%). In this group, memory function and executive function were significantly reduced.
Conclusions:
Patients treated with extracorporeal membrane oxygenation for respiratory failure may have normal cognitive function years after treatment, if not affected by cerebrovascular lesions. Permissive hypoxemia was not correlated with long-term cognitive dysfunction in the present study. Further prospective studies with minimal loss to follow-up are direly needed to confirm our findings.
Prédiction de la mortalité chez les patients traités par ECMO après un syndrome coronarien aigu
Pabst et al., CCM, 2018
Objectives:
Acute myocardial infarction is the most common cause of cardiogenic shock. Although the number of patients with acute myocardial infarction complicated by cardiogenic shock who were treated with venoarterial extracorporeal membrane oxygenation increased during the last decade, detailed data on survival are lacking. We sought to analyze covariates that were independently associated with survival in this patient population and to externally validate the newly developed prEdictioN of Cardiogenic shock OUtcome foR Acute myocardial infarctionpatients salvaGed by venoarterial Extracorporeal membrane oxygenation (ENCOURAGE) score.
Design:
Retrospective clinical study.
Setting:
A single academic teaching hospital.
Patients:
Adult patients with acute myocardial infarction complicated by cardiogenic shock who were supported by venoarterial extracorporeal membrane oxygenation from June 2008 to September 2016.
Interventions:
Fourteen individual variables were assessed for their association with the primary endpoint. These variables were prespecified by the study team as being the most likely to affect survival. A receiver operating characteristic analysis was also performed to test the ability of the ENCOURAGE score to predict survival in this patient cohort.
Measurements and Main Results:
The primary endpoint of the study was in-hospital survival. A total of 61 patients were included in the analysis. Thirty-seven (60.7%) could be weaned from venoarterial extracorporeal membrane oxygenation and 36 (59.0%) survived. Survival was significantly higher in patients less than 65 years old (odds ratio, 14.6 [CI, 2.5–84.0]; p = 0.003), whose body mass index was less than 32 kg/m2 (odds ratio, 5.5 [CI, 1.2–25.4]; p = 0.029) and international normalized ratio was less than 2 (odds ratio, 7.3 [CI, 1.3–40.1]; p = 0.022). In patients where the first lactate drawn was less than 3 mmol/L, the survival was not significantly higher (odds ratio, 4.4 [CI, 0.6–32.6]; p = 0.147). The C-statistic for predicting survival using a modified version of the ENCOURAGE score, which replaced prothrombin activity less than 50% with an international normalized ratio greater than 2, was 0.74 (95% CI, 0.61–0.87).
Conclusions:
In this single-center study, several important covariates were associated with improved survival in patients with acute myocardial infarction complicated by cardiogenic shock who were supported by venoarterial extracorporeal membrane oxygenation and the ENCOURAGE score was found to be externally valid for predicting survival to hospital discharge.
Méta-analyse sur les vasopresseurs à utiliser dans l’arrêt cardiaque, l’Adrénaline est-elle toujours l’amine de premier choix ?
Méta-analyse sur la gestion de l’antibiothérapie guidée par la PCT
Lam et al., CCM, 2018
La concentration expirée d’halogéné sous-estime-t-elle l’effet second gaz alvéolaire ? Une modélisation mathématique
Can Mathematical Modeling Explain the Measured Magnitude of the Second Gas Effect?
Ben Korman, M.D.; et al., Anesthesiology 2018, Vol.128, 1075-1083.
doi:10.1097/ALN.
Background:
Methods:
Results:
Conclusions:
L’infarctus post-opératoire après chirurgie non-cardiaque est majoritairement de type II
Etiology of Acute Coronary Syndrome after Noncardiac Surgery
doi:10.1097/ALN.
Background:
Methods:
Results:
Conclusions:
La lidocaïne inhibe la migration leucocytaire. Une cible thérapeutique ?
Sodium Channel Nav1.3 Is Expressed by Polymorphonuclear Neutrophils during Mouse Heart and Kidney Ischemia InVivo and Regulates Adhesion, Transmigration, and Chemotaxis of Human and Mouse Neutrophils In Vitro
Marit Poffers, et al., Anesthesiology 2018,
doi:10.1097/ALN.
Background:
Methods:
Results:
Conclusions:
Le non accès à l’analgésie péridurale au cours du travail obstétrical influence-t-il le développement de dépression du post-partum ? Non d’après une étude prospective
Orbach-Zinger,et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002501
BACKGROUND:
Postpartum depression (PPD) is associated with pain during and after delivery, with studies showing reduced rates among women delivering with labor epidural analgesia (LEA). We hypothesized that women who intend to deliver with LEA but do not receive it are at higher risk for PPD at 6 weeks due to the combined experience of untreated labor pain and unmatched expectations during labor, and evaluated the interaction between labor plans related to LEA, satisfaction with pain control when actually delivering with LEA, and PPD at 6 weeks after delivery.
METHODS:
A total of 1497 women with a vaginal delivery were enrolled into this prospective longitudinal study. Women’s initial intention to deliver with or without LEA, how they subsequently delivered, and satisfaction with pain relief were recorded on postpartum day 1. Primary aim was selected as PPD at 6 weeks among women intending to deliver with but subsequently delivering without LEA compared with the rest of the cohort. Primary outcome was PPD at 6 weeks using the Edinburgh Postnatal Depression Scale; PPD was defined with a score ≥10 (scale from 0 to 30). Demographic and obstetric data were recorded. Fisher exact test was used for comparisons between groups. The interaction between intention and actual delivery with regard to LEA and PPD was tested.
RESULTS:
Overall, 87 of 1326 women completing the study at 6 weeks had PPD (6.6%). For the primary aim, 439 (29.3%) delivered without LEA, of which 193 (12.9%) had intended to deliver with LEA; the PPD rate among these women was 8.1%, which was not statistically different from the rest of the cohort (6.3%; odds ratio [OR], 1.30; 95% confidence interval [CI], 0.72–2.38; P = .41). A total of 1058 women (70.7%) delivered with LEA and 439 (29.3%) delivered without; therefore, 1169 (78.1%) delivered as intended and 328 (21.9%) did not (unmatched expectations). Evaluating the interaction between effects, there was a strong negative additive interaction between intending to deliver without LEA and actually delivering with LEA (risk difference = −8.6%, 95% CI, 16.2%–1.6%; P = .014) suggesting that unmatched intention effect is significantly associated with negative outcome. In multiple regression analysis, while intending to deliver with LEA (OR, 1.06; 95% CI, 1.01–1.11; P = .029) and actually delivering with LEA (OR, 1.07; 95% CI, 1.01–1.13; P = .018) both increased the odds for PPD, the multiplicative interaction was protective (OR, 0.92; 95% CI, 0.86–0.99; P = .022), after adjusting for cofactors.
CONCLUSIONS:
Our study results did not demonstrate a significant increase in the odds for PPD at 6 weeks among women who intended to deliver with LEA but subsequently delivered without. However, we identified a protective interaction between intended LEA use and actual use on the incidence of PPD. Our data suggest an increased risk when women do not deliver as intended, particularly when not initially intending to deliver with LEA. The relationship between unplanned LEA and PPD may be mediated by a physically difficult delivery rather than or in addition to negative emotions related to unmet expectations or a sense of personal failure; therefore, counseling women after delivery to address any negative perceptions may be useful.
Lors de l’intubation Nasotrachéale, l’utilisation d’une Bougie d’Eishmann permet de réduire le saignement, le recours à l’utilisation d’une Magill et la durée de l’intubation.
Pourfakhr et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002853
BACKGROUND:
Nasotracheal intubation is commonly performed to provide a secure airway for the maintenance of general anesthesia in maxillofacial surgeries. Routine nasotracheal intubation is performed under general anesthesia by direct laryngoscopy, frequently with the aid of Magill forceps. This method can be time-consuming and may cause bleeding in the field of view. A gum elastic bougie (GEB) is a cheap, slender, and flexible device that could expedite nasotracheal intubation. The aim of this study was to evaluate the use of a GEB during nasotracheal intubation to facilitate the procedure and reduce the rate of complications.
METHODS:
In this randomized clinical trial study, 110 patients with American Society of Anesthesiologists (ASA) physical status I–II from 15 to 65 years of age were randomized into 2 equal groups. In both groups, a GlideScope and armored tube were used. In the GEB group, GEB was used to facilitate nasal intubation while the nasal intubation was performed without the aid of GEB in the routine group. The difficult intubation (defined as >1 attempt for intubation) was the primary outcome, and the duration of the intubation, the presence of traces of bleeding, the need for a tube replacement, and the usage of Magill forceps were the secondary outcomes.
RESULTS:
The incidence of bleeding in the GEB group was 1.81% vs 43.63% in the routine group (P < .001). In 5.5% of the GEB group, Magill forceps were used to advance the tube versus 67.3% in the routine group (P < .001). The mean time for intubation in GEB group was 48.63 ± 8.53 vs 55.9 ± 10.76 seconds in the routine group (P < .001).
CONCLUSIONS:
The GEB is a useful aid to nasotracheal intubation, reducing bleeding, the requirement for Magill forceps and, to a small degree, intubation time. A case exists for its routine use for this purpose.
Management périopératoire et survie au cours de la chirurgie pour cancer pulmonaire : étude rétrospective sur les facteurs de risques et les facteurs protecteurs.
Huang et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002886
BACKGROUND:
Surgical resection is the main treatment for patients with non–small-cell lung cancer (NSCLC), but patients’ long-term outcome is still challenging. The purpose of this study was to identify predictors of long-term survival in patients after lung cancer surgery.
METHODS:
Patients who underwent surgery for NSCLC from January 1, 2006, to December 31, 2009, were enrolled into this retrospective cohort study. The primary outcome was the survival length after surgery. Predictors of long-term survival were screened with the multivariable Cox proportional hazard model.
RESULTS:
Postoperative follow-up was completed in 588 patients with a median follow-up duration of 5.2 years (interquartile range, 2.0–6.8). Two hundred ninety-one patients (49.5%) survived at the end of follow-up with median survival duration of 64.3 months (interquartile range, 28.5–81.6). The overall survival rates were 90.8%, 70.0%, and 57.1% at the end of the first, third, and fifth year after surgery, respectively. Limited resection (hazard ratio [HR], 1.46; 95% confidence interval [CI], 1.08–1.98; P = .013) and large tumor size (HR, 1.29; 95% CI, 1.17–1.42; P < .001) were associated with short survival; whereas high body mass index grade (HR, 0.82; 95% CI, 0.69–0.97; P = .021), highly differentiated tumor (HR, 0.59; 95% CI, 0.37–0.93; P = .024), dissection of mediastinal lymph node during surgery (HR, 0.45; 95% CI, 0.30–0.67; P < .001), and perioperative use of dexamethasone (HR, 0.70; 95% CI, 0.54–0.90; P = .006) were associated with long survival. No association was found between perioperative use of flurbiprofen axetil and long survival (HR, 0.80; 95% CI, 0.62–1.03; P = .086). However, combined administration of dexamethasone and flurbiprofen axetil was associated with longer survival (compared to no use of both: adjusted HR, 0.57; 95% CI, 0.38–0.84; P = .005).
CONCLUSIONS:
Certain factors in particular perioperative dexamethasone and flurbiprofen axetil therapy may improve patients’ long-term survival after surgery for NSCLC. Given the small sample size, these findings should be interpreted with caution, and randomized clinical trials are needed for further clarification.
Méta-analyse sur l’ALR périphérique au cours des fractures de hanche :
Réduction de la douleur à la mobilisation, du risque de pneumopathie nosocomiale, de la durée avant 1ère mobilisation et des coûts.
Guay et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002489
Revue sur l’interaction entre les colloïdes et la microcirculation
He et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002620
L’anaphylaxie au Sugammadex est-elle aussi fréquente que celle à la Celocurine ?
Miyazaki et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002562
Revue sur le risque de douleur après césarienne
Gamez et al., Anesthesia & Analgesia, 2018
doi: 10.1213/ANE.0000000000002658





 5 juin 2018
5 juin 2018









 Étiquettes :
Étiquettes :