Biblio du mois : Septembre 2018
Après un congrès SFAR 2018 bien fameux où l’AJAR Paris a répondu présent, nous vous invitons à profiter de la nouvelle biblio du mois !
Avec entre (beaucoup) d’autres, une grosse étude du JAMA sur le Burn-out et les Remords des internes en Médecine (aux USA), mais aussi de l’hémato avec de la gestion d’anémie pré-opératoire et sur la physiologie de l’anémie liée au trauma. On apprécie les études rassurantes sur les corticoïdes sur la curarisation et l’impact sur les neuropathies de réanimation sauf pour la grippe.
On n’oublie pas les recommandations sur la prévention et la gestion de la douleur, agitation, délirium et sommeil en réanimation mais aussi de vous rappeler que l’AJAR Paris co-organise avec l’ESRA France une journée de formation à l’ALR (au sein d’un circuit entier de formations pour se perfectionner) : https://www.ajar-online.fr/formation-alr-journee-de-formation-esra-france-tour/
Malgré une antibiothérapie peu recommandable, il serait possible de traiter les appendicites non compliquées par traitement médical : on va pouvoir se reposer un peu plus en garde ?
Dans tous les cas, attention au Burn-out ! et Si vous avez besoin les liens pour obtenir de l’aide sont ici.
Trêve d’edito : Let’s Biblio !
Des commentaires sur EOLIA !
NEJM 2018
10.1056/NEJMc1808731
https://www.nejm.org/doi/full/10.1056/NEJMc1808731
Une revue sur le rejet humoral des transplants solides
Antibody-Mediated Rejection of Solid-Organ Allografts
Alexandre Loupy et Carmen Lefaucheur, NEJM, 2018
10.1056/NEJMra1802677
https://www.nejm.org/doi/full/10.1056/NEJMra1802677
Abstract
This review focuses on current standards for management of antibody-mediated rejection in solid-organ transplant recipients and emphasizes advances that may ultimately lead to the development of precise, pathogenesis-based therapeutic approaches.
Etude sur le Burn-out et Remords par spécialité : Encore du travail !
https://jamanetwork.com/journals/jama/article-abstract/2702870
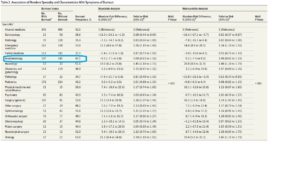
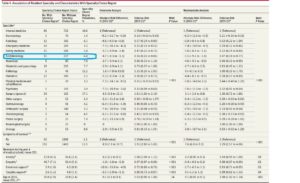
Importance Burnout among physicians is common and has been associated with medical errors and lapses in professionalism. It is unknown whether rates for symptoms of burnout among resident physicians vary by clinical specialty and if individual factors measured during medical school relate to the risk of burnout and career choice regret during residency.
Objective To explore factors associated with symptoms of burnout and career choice regret during residency.
Design, Setting, and Participants Prospective cohort study of 4732 US resident physicians. First-year medical students were enrolled between October 2010 and January 2011 and completed the baseline questionnaire. Participants were invited to respond to 2 questionnaires; one during year 4 of medical school (January-March 2014) and the other during the second year of residency (spring of 2016). The last follow-up was on July 31, 2016.
Exposures Clinical specialty, demographic characteristics, educational debt, US Medical Licensing Examination Step 1 score, and reported levels of anxiety, empathy, and social support during medical school.
Main Outcomes and Measures Prevalence during second year of residency of reported symptoms of burnout measured by 2 single-item measures (adapted from the Maslach Burnout Inventory) and an additional item that evaluated career choice regret (defined as whether, if able to revisit career choice, the resident would choose to become a physician again).
Results Among 4696 resident physicians, 3588 (76.4%) completed the questionnaire during the second year of residency (median age, 29 [interquartile range, 28.0-31.0] years in 2016; 1822 [50.9%] were women). Symptoms of burnout were reported by 1615 of 3574 resident physicians (45.2%; 95% CI, 43.6% to 46.8%). Career choice regret was reported by 502 of 3571 resident physicians (14.1%; 95% CI, 12.9% to 15.2%). In a multivariable analysis, training in urology, neurology, emergency medicine, and general surgery were associated with higher relative risks (RRs) of reported symptoms of burnout (range of RRs, 1.24 to 1.48) relative to training in internal medicine. Characteristics associated with higher risk of reported symptoms of burnout included female sex (RR, 1.17 [95% CI, 1.07 to 1.28]; risk difference [RD], 7.2% [95% CI, 3.1% to 11.3%]) and higher reported levels of anxiety during medical school (RR, 1.08 per 1-point increase [95% CI, 1.06 to 1.11]; RD, 1.8% per 1-point increase [95% CI, 1.6% to 2.0%]). A higher reported level of empathy during medical school was associated with a lower risk of reported symptoms of burnout during residency (RR, 0.99 per 1-point increase [95% CI, 0.99 to 0.99]; RD, −0.5% per 1-point increase [95% CI, −0.6% to −0.3%]). Reported symptoms of burnout (RR, 3.20 [95% CI, 2.58 to 3.82]; RD, 15.0% [95% CI, 12.8% to 17.3%]) and clinical specialty (range of RRs, 1.66 to 2.60) were both significantly associated with career choice regret.
Conclusions and Relevance Among US resident physicians, symptoms of burnout and career choice regret were prevalent, but varied substantially by clinical specialty. Further research is needed to better understand these differences and to address these issues.
Revue sur le Burn-out : de 0 à 80 % de prévalence…
https://jamanetwork.com/journals/jama/article-abstract/2702871
Appendicite non compliquée : pas une urgence chirurgicale ?
= 39% de récurrence à 5ans par traitement médical
https://jamanetwork.com/journals/jama/article-abstract/2703354
Du fer oral ou intraveineux avec l’EPO pour corriger l’anémie pré-opératoire en chirurgie orthopédique ?
Biboulet et al, Anesthesiology, 2018
10.1097/ALN.0000000000002376
http://anesthesiology.pubs.asahq.org/article.aspx?articleid=2696585
Abstract
Editor’s Perspective:
What We Already Know about This Topic:
Epoetin-α is often given to patients scheduled for major orthopedic surgery
It remains unknown whether it is best to accompany epoetin-α with oral or intravenous iron
What This Article Tells Us That Is New:
Hemoglobin level the day before surgery was 1 g/dl greater in 50 patients randomized to intravenous iron than in those assigned to oral iron
About half the patients given oral iron reported gastrointestinal symptoms
Intravenous iron is preferable to oral iron as a supplement to epoetin-α
Background: Preoperative administration of epoetin-α with iron is commonly used in anemic patients undergoing major orthopedic surgery, but the optimal route of iron intake is controversial. The aim of this study was to compare the clinical effects of erythropoietin in combination with oral or intravenous iron supplementation.
Methods: This study was a prospective, randomized, single-blinded, parallel arm trial. Patients scheduled for elective hip or knee arthroplasty with hemoglobin 10 to 13 g/dl received preoperative injections of erythropoietin with oral ferrous sulfate or intravenous ferric carboxymaltose. The primary endpoint was the hemoglobin value the day before surgery.
Results: One hundred patients were included in the analysis. The day before surgery, hemoglobin, increase in hemoglobin, and serum ferritin level were higher in the intravenous group. For the intravenous and oral groups, respectively, hemoglobin was as follows: median, 14.9 g/dl (interquartile range, 14.1 to 15.6) versus 13.9 g/dl (interquartile range, 13.2 to 15.1), group difference, 0.65 g/dl (95% CI, 0.1 to 1.2; P = 0.017); increase in hemoglobin: 2.6 g/dl (interquartile range, 2.1 to 3.2) versus 1.9 g/dl (interquartile range, 1.4 to 2.5), group difference, 0.7 g/dl (95% CI, 0.3 to 1.1; P < 0.001); serum ferritin: 325 µg/l (interquartile range, 217 to 476) versus 64.5 µg/l (interquartile range, 44 to 107), group difference, 257 µg/l (95% CI, 199 to 315; P < 0.001). The percentage of patients with nausea, diarrhea, or constipation was higher in the oral group, 52% versus 2%; group difference, 50% (95% CI, 35 to 64%; P < 0.0001).
Conclusions: After preoperative administration of erythropoietin, body iron stores and stimulation of the erythropoiesis were greater with intravenous ferric carboxymaltose than with oral ferrous sulfate supplementation.
Suivi des familles après décision de don d’organes en réanimation
Physiologie de l’anémie associée au trauma
Revue sur l’embolie pulmonaire massive
Moins de dysfonction cognitive post-opératoire lors d’une anesthésie générale au Propofol vs Sevoflurane chez le sujet âgé ?
Prédiction de la réponse au remplissage chez le patient en ventilation spontanée avec le doppler carotidien
Édition spéciale sur les interactions cœur-poumons :
Dosage élevé du sRAGE associé à une surmortalité ARDS ?
Plasma sRAGE is independently associated with increased mortality in ARDS: a meta-analysis of individual patient data
doi: 10.1007/s00134-018-5327-1
Purpose
The soluble receptor for advanced glycation end-products (sRAGE) is a marker of lung epithelial injury and alveolar fluid clearance (AFC), with promising values for assessing prognosis and lung injury severity in acute respiratory distress syndrome (ARDS). Because AFC is impaired in most patients with ARDS and is associated with higher mortality, we hypothesized that baseline plasma sRAGE would predict mortality, independently of two key mediators of ventilator-induced lung injury.
Methods
We conducted a meta-analysis of individual data from 746 patients enrolled in eight prospective randomized and observational studies in which plasma sRAGE was measured in ARDS articles published through March 2016. The primary outcome was 90-day mortality. Using multivariate and mediation analyses, we tested the association between baseline plasma sRAGE and mortality, independently of driving pressure and tidal volume.
Results
Higher baseline plasma sRAGE [odds ratio (OR) for each one-log increment, 1.18; 95% confidence interval (CI) 1.01–1.38; P = 0.04], driving pressure (OR for each one-point increment, 1.04; 95% CI 1.02–1.07; P = 0.002), and tidal volume (OR for each one-log increment, 1.98; 95% CI 1.07–3.64; P = 0.03) were independently associated with higher 90-day mortality in multivariate analysis. Baseline plasma sRAGE mediated a small fraction of the effect of higher Δ P on mortality but not that of higher V _T.
Conclusions
Higher baseline plasma sRAGE was associated with higher 90-day mortality in patients with ARDS, independently of driving pressure and tidal volume, thus reinforcing the likely contribution of alveolar epithelial injury as an important prognostic factor in ARDS. Registration: PROSPERO (ID: CRD42018100241).
Grippe ou corticoïdes, il faut choisir :
Corticosteroid treatment in critically ill patients with severe influenza pneumonia: a propensity score matching study
doi: 10.1007/s00134-018-5332-4
Purpose
To determine clinical predictors associated with corticosteroid administration and its association with ICU mortality in critically ill patients with severe influenza pneumonia.
Methods
Secondary analysis of a prospective cohort study of critically ill patients with confirmed influenza pneumonia admitted to 148 ICUs in Spain between June 2009 and April 2014. Patients who received corticosteroid treatment for causes other than viral pneumonia (e.g., refractory septic shock and asthma or chronic obstructive pulmonary disease [COPD] exacerbation) were excluded. Patients with corticosteroid therapy were compared with those without corticosteroid therapy. We use a propensity score (PS) matching analysis to reduce confounding factors. The primary outcome was ICU mortality. Cox proportional hazards and competing risks analysis was performed to assess the impact of corticosteroids on ICU mortality.
Results
A total of 1846 patients with primary influenza pneumonia were enrolled. Corticosteroids were administered in 604 (32.7%) patients, with methylprednisolone the most frequently used corticosteroid (578/604 [95.7%]). The median daily dose was equivalent to 80mg of methylprednisolone (IQR 60–120) for a median duration of 7 days (IQR 5–10). Asthma, COPD, hematological disease, and the need for mechanical ventilation were independently associated with corticosteroid use. Crude ICU mortality was higher in patients who received corticosteroids (27.5%)than in patients who did not receive corticosteroids (18.8%, p<0.001). After PS matching, corticosteroid use was associated with ICU mortality in the Cox (HR = 1.32 [95% CI 1.08–1.60], p<0.006) and competing risks analysis (SHR = 1.37 [95% CI 1.12–1.68], p = 0.001).
Conclusion
Administration of corticosteroids in patients with severe influenza pneumonia is associated with increased ICU mortality, and these agents should not be used as co-adjuvant therapy.
Purpura fulminans, quel pronostic ?
Clinical spectrum and short-term outcome of adult patients with purpura fulminans: a French multicenter retrospective cohort study
doi: 10.1007/s00134-018-5341-3
Purpose
Data on purpura fulminans (PF) in adult patients are scarce and mainly limited to meningococcal infections. Our aim has been to report the clinical features and outcomes of adult patients admitted in the intensive care unit (ICU) for an infectious PF, as well as the predictive factors for limb amputation and mortality.
Methods
A 17-year national multicenter retrospective cohort study in 55 ICUs in France from 2000 to 2016, including adult patients admitted for an infectious PF defined by a sudden and extensive purpura, together with the need for vasopressor support. Primary outcome variables included hospital mortality and amputation during the follow-up period (time between ICU admission and amputation, death or end of follow-up).
Results
Among the 306 included patients, 126 (41.2%; 95% CI 35.6–46.9) died and 180 (58.8%; 95% CI 53.3–64.3) survived during the follow-up period [13 (3–24) days], including 51/180 patients (28.3%, 95% CI 21.9–35.5) who eventually required limb amputations, with a median number of 3 (1–4) limbs amputated. The two predominantly identified microorganisms were Neisseria meningitidis (63.7%) and Streptococcus pneumoniae (21.9%). By multivariable Cox model, SAPS II [hazard-ratio (HR) = 1.03 (1.02–1.04); p<0.001], lower leucocytes [HR 0.83 (0.69–0.99); p = 0.034] and platelet counts [HR 0.77 (0.60–0.91); p = 0.007], and arterial blood lactate levels [HR 2.71 (1.68–4.38); p<0.001] were independently associated with hospital death, while a neck stiffness [HR 0.51 (0.28–0.92); p = 0.026] was a protective factor. Infection with Streptococcus pneumoniae [sub-hazard ratio 1.89 (1.06–3.38); p = 0.032], together with arterial lactate levels and ICU admission temperature, was independently associated with amputation by a competing risks analysis.
Conclusion
Purpura fulminans carries a high mortality and morbidity. Pneumococcal PF leads to a higher risk of amputation.
Revue sur la tropininémie pre-opératoire
Une durée d’action diminuée chez les BMI <25 ?
BACKGROUND The duration of rocuronium in patients with BMI more than 30 kg m−2 is prolonged. Whether the reverse is true when BMI is less than 18.5 kg m−2 is unclear.
OBJECTIVE The objective of this study was to investigate whether a BMI less than 25 kg m−2 affects the duration of rocuronium in doses adjusted for actual body weight.
DESIGN A prospective, observational, single-centre study.
SETTING The operating room of a teaching hospital from 1 June 2008 to 30 June 2015.
PATIENTS Thirty patients with American Society of Anesthesiologists physical status I or II who were scheduled to undergo elective surgery (BMI < 25 kg m−2, aged 23 to 74 years) maintained by 0.7 minimum alveolar concentration sevoflurane and remifentanil.
MAIN OUTCOME MEASURES Repetitive train-of-four stimulation was applied and contractions of the adductor pollicis muscle were recorded. Duration of the initial dose of rocuronium (D1) was defined as the time from injection of rocuronium 0.6 mg kg−1 to return of first twitch height to 25% of the control. Duration of additional doses (D2) was the time from a supplement of 0.15 mg kg−1 rocuronium to return of first twitch height to 25% of the control. The relationship between D1 or D2 and BMI was examined using linear regression analysis.
RESULTS Linear regression analysis revealed a significant correlation between duration of initial dose and BMI (R2 = 0.246; P = 0.00531). A significant correlation between the duration of the additional dose and BMI was also found (R 2 = 0.316; P = 0.00122).
CONCLUSION The lower the BMI, the shorter the duration of rocuronium at initial and additional doses determined by the actual body weight in adult patients with a BMI less than 25 kg m−2.
Pas d’effet des corticoïdes sur la curarisation par Rocuronium et son antagonisation ?
Méta-analyse sur la Dexmedetomidine en ALR
Efficacy and safety of dexmedetomidine in peripheral nerve blocks: A meta-analysis and trial sequential analysis
Une diminution de l’expression du récepteur aux glucocorticoïdes dans les leucocytes circulants est associée à une évolution défavorable au cours du sepsis pédiatrique
Alder MN et al, Critical Care, 2018
10.1186/s13054-018-2177-8
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2177-8
Abstract
Background
There is controversy around the prescription of adjunct corticosteroids in patients with fluid-refractory septic shock, and studies provide mixed results, showing benefit, no benefit, and harm. Traditional means for evaluating whether a patient receives corticosteroids relied on anecdotal experience or measurement of serum cortisol production following stimulation. We set out to measure both serum cortisol and the intracellular signaling receptor for cortisol, the glucocorticoid receptor (GCR), in this group of patients.
Methods
We enrolled pediatric patients admitted to the pediatric intensive care unit with a diagnosis of systemic inflammatory response syndrome (SIRS), sepsis, or septic shock as well as healthy controls. We measured serum cortisol concentration and GCR expression by flow cytometry in peripheral blood leukocytes on the day of admission and day 3.
Results
We enrolled 164 patients for analysis. There was no difference between GCR expression comparing SIRS, sepsis, and septic shock. When all patients with septic shock were compared, those patients with a complicated course, defined as two or more organ failures at day 7 or death by day 28, had lower expression of GCR in all peripheral blood leukocytes. Further analysis suggested that patients with the combination of low GCR and high serum cortisol had higher rates of complicated course (75%) compared with the other three possible combinations of GCR and cortisol levels: low GCR and low cortisol (33%), high GCR and high cortisol (33%), and high GCR and low cortisol (13%; P <0.05).
Conclusions
We show that decreased expression of the GCR correlated with poor outcome from septic shock, particularly in those patients with high serum cortisol. This is consistent with findings from transcriptional studies showing that downregulation of GCR signaling genes portends worse outcome.
L’expression monocytaire du HLA-DR utile pour distinguer un syndrome hémophagocytaire d’un sepsis ?
Remy et al, Critical Care, 2018
10.1186/s13054-018-2146-2
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2146-2
Deux profils d’échec d’extubation avec des facteurs de risque communs et spécifiques
Jaber et al, Critical care, 2018
10.1186/s13054-018-2150-6
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2150-6
Abstract
Background
Patients liberated from invasive mechanical ventilation are at risk of extubation failure, including inability to breathe without a tracheal tube (airway failure) or without mechanical ventilation (non-airway failure). We sought to identify respective risk factors for airway failure and non-airway failure following extubation.
Methods
The primary endpoint of this prospective, observational, multicenter study in 26 intensive care units was extubation failure, defined as need for reintubation within 48 h following extubation. A multinomial logistic regression model was used to identify risk factors for airway failure and non-airway failure.
Results
Between 1 December 2013 and 1 May 2015, 1514 patients undergoing extubation were enrolled. The extubation-failure rate was 10.4% (157/1514), including 70/157 (45%) airway failures, 78/157 (50%) non-airway failures, and 9/157 (5%) mixed airway and non-airway failures. By multivariable analysis, risk factors for extubation failure were either common to airway failure and non-airway failure: intubation for coma (OR 4.979 (2.797–8.864), P < 0.0001 and OR 2.067 (1.217–3.510), P = 0.003, respectively, intubation for acute respiratory failure (OR 3.395 (1.877–6.138), P < 0.0001 and OR 2.067 (1.217–3.510), P = 0.007, respectively, absence of strong cough (OR 1.876 (1.047–3.362), P = 0.03 and OR 3.240 (1.786–5.879), P = 0.0001, respectively, or specific to each specific mechanism: female gender (OR 2.024 (1.187–3.450), P = 0.01), length of ventilation > 8 days (OR 1.956 (1.087–3.518), P = 0.025), copious secretions (OR 4.066 (2.268–7.292), P < 0.0001) were specific to airway failure, whereas non-obese status (OR 2.153 (1.052–4.408), P = 0.036) and sequential organ failure assessment (SOFA) score ≥ 8 (OR 1.848 (1.100–3.105), P = 0.02) were specific to non-airway failure. Both airway failure and non-airway failure were associated with ICU mortality (20% and 22%, respectively, as compared to 6% in patients with extubation success, P < 0.0001).
Conclusions
Specific risk factors have been identified, allowing us to distinguish between risk of airway failure and non-airway failure. The two conditions will be managed differently, both for prevention and curative strategies.
L’ECMO, une option non déraisonnable pour l’insuffisance respiratoire aiguë des enfants en cours d’induction d’une leucémie aiguë ?
Cortina et al, Critical care, 2018
10.1186/s13054-018-2134-6
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2134-6
« Hypervolémie » et « surcharge hydrique », des termes interchangeables ?
Vincent et al, Critical Care, 2018
10.1186/s13054-018-2141-7
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2141-7
Pour ou contre l’utilisation d’algorithmes informatique pour programmer la ventilation mécanique ?
Oui : https://journal.chestnet.org/#/article/S0012-3692(18)30926-7/fulltext
Non : https://journal.chestnet.org/#/article/S0012-3692(18)30932-2/fulltext
Complication pulmonaire post-opératoire chez les patients toxicomanes
BACKGROUND: As the rate of opioid use disorders continues to rise, perioperative physicians are increasingly faced with the challenge of providing analgesia to these patients after surgery. Due to the likelihood of opioid dose escalation in the perioperative period, we hypothesized that opioid-dependent patients would be at increased risk for postoperative pulmonary complications.
METHODS: A retrospective cross-sectional analysis of patients undergoing 6 representative elective surgical procedures was performed using the Nationwide Inpatient Sample from 2002 to 2011. The primary outcome was a composite including prolonged mechanical ventilation, reintubation, and acute respiratory failure. Secondary outcomes were length of stay, in-hospital mortality, and total hospital costs. Both multivariable logistic regression and propensity score matching were used to determine the impact of opioid use disorder on outcomes.
RESULTS: The total sample-weighted cohort consisted of 7,533,050 patients. Patients with opioid use disorders were more likely to suffer pulmonary complications, with a frequency of 4.2% compared to 1.6% in the nonopioid-dependent group (P < .001), and had a 1.62 times higher odds (95% confidence interval [CI], 1.16–2.27) in multivariable regression analysis. In a secondary subgroup analysis, only patients undergoing a colectomy had a greater odds of suffering pulmonary complications (odds ratio, 2.64; 95% CI, 1.42–4.91; P = .0021). Additionally, patients with an opioid use disorder had a longer length of stay (0.84 days [95% CI, 0.52–1.16; P < .001]) and greater costs ($1816 [95% CI, 935–2698; P < .001]).
CONCLUSIONS: This study demonstrates that patients with opioid use disorders are at increased risk for postoperative pulmonary complications, and have prolonged length of stay and resource utilization. Further research is needed regarding interventions to reduce the risk of complications in this subset of patients.
Impact de l’anesthésie locorégionale dans le pronostic du cancer gastrique ?
Regional anesthesia may play a beneficial role in long-term oncological outcomes.
Specifically, it has been suggested that it can prolong recurrence-free survival and overall survival after gastrointestinal cancer surgery, including gastric and esophageal cancer, by modulating the immune and inflammatory response. However, the results from human studies are conflicting. The goal of this systematic review was to summarize the evidence on the impact of regional anesthesia on immunomodulation and cancer recurrence after gastric and esophageal surgery.
We conducted a literature search of 5 different databases. Two independent reviewers analyzed the quality of the selected manuscripts according to prespecified inclusion and exclusion criteria. Randomized controlled trials were assessed for potential sources of bias by using the Cochrane Risk of Bias tool. A total of 6 studies were included in the quality analysis and systematic review. A meta-analysis was not conducted for several reasons, including high heterogeneity among studies, low quality of the reports, and lack of standardized outcomes definitions.
Although the literature suggests that regional anesthesia has some modulatory effects on the inflammatory and immunological response in the studied patient population, our systematic review indicates that there is no evidence to support or refute the use of epidural anesthesia or analgesia with the goal of reducing cancer recurrence after gastroesophageal cancer surgery.
Apnée du sommeil, STOP-Bang, oxymétrie ou les 2 pour le screening des patients en pré-opératoire ?
BACKGROUND: Obstructive sleep apnea (OSA) is related to postoperative complications and is a common disorder. Most patients with sleep apnea are, however, undiagnosed, and there is a need for simple screening tools. We aimed to investigate whether STOP-Bang and oxygen desaturation index can identify subjects with OSA.
METHODS: In this prospective, observational multicenter trial, 449 adult patients referred to a sleep clinic for evaluation of OSA were investigated with ambulatory polygraphy, including pulse oximetry and the STOP-Bang questionnaire in 4 Swedish centers. The STOP-Bang score is the sum of 8 positive answers to Snoring, Tiredness, Observed apnea, high blood Pressure, Body mass index >35 kg/m2, Age >50 years, Neck circumference >40 cm, and male Gender.
RESULTS: The optimal STOP-Bang cutoff score was 6 for moderate and severe sleep apnea, defined as apnea-hypopnea index (AHI) ≥15, and the sensitivity and specificity for this score were 63% (95% CI, 0.55–0.70) and 69% (95% CI, 0.64–0.75), respectively. A STOP-Bang score of <2 had a probability of 95% (95% CI, 0.92–0.98) to exclude an AHI >15 and a STOP-Bang score of ≥6 had a specificity of 91% (95% CI, 0.87–0.94) for an AHI >15. The items contributing most to the STOP-Bang were the Bang items. There was a positive correlation between AHI versus STOP-Bang and between AHI versus oxygen desaturation index, Spearman ρ 0.50 (95% CI, 0.43–0.58) and 0.96 (95% CI, 0.94–0.97), respectively.
CONCLUSIONS: STOP-Bang and pulse oximetry can be used to screen for sleep apnea. A STOP-Bang score of <2 almost excludes moderate and severe OSA, whereas nearly all the patients with a STOP-Bang score ≥6 have OSA. We suggest the addition of nightly pulse oximetry in patients with a STOP-Bang score of 2–5 when there is a need for screening for sleep apnea (ie, before surgery).
Allergie aux betalactamines, ce que l’anesthésiste doit savoir :
Administration of preoperative antimicrobial prophylaxis, often with a cephalosporin, is the mainstay of surgical site infection prevention guidelines. Unfortunately, due to prevalent misconceptions, patients labeled as having a penicillin allergy often receive alternate and less-effective antibiotics, placing them at risk of a variety of adverse effects including increased morbidity and higher risk of surgical site infection.
The perioperative physician should ascertain the nature of previous reactions to aid in determining the probability of the prevalence of a true allergy. Penicillin allergy testing may be performed but may not be feasible in the perioperative setting. Current evidence on the structural determinants of penicillin and cephalosporin allergies refutes the misconception of cross-reactivity between penicillins and cefazolin, and there is no clear evidence of an increased risk of anaphylaxis in cefazolin-naive, penicillin-allergic patients.
A clinical practice algorithm for the perioperative evaluation and management of patients reporting a history of penicillin allergy is presented, concluding that cephalosporins can be safely administered to a majority of such patients
Physiologie et conséquence des doubles déclenchements en ventilation mécanique
Meilleur pronostic mais plus de polyneuromyopathie lors de l’utilisation de corticoïdes dans le choc septique ? Revue et méta-analyse
Recommandations sur la prévention et la gestion de la douleur, agitation, délirium et sommeil en réanimation





 3 octobre 2018
3 octobre 2018











 Étiquettes :
Étiquettes :